Table of Contents
True vertigo
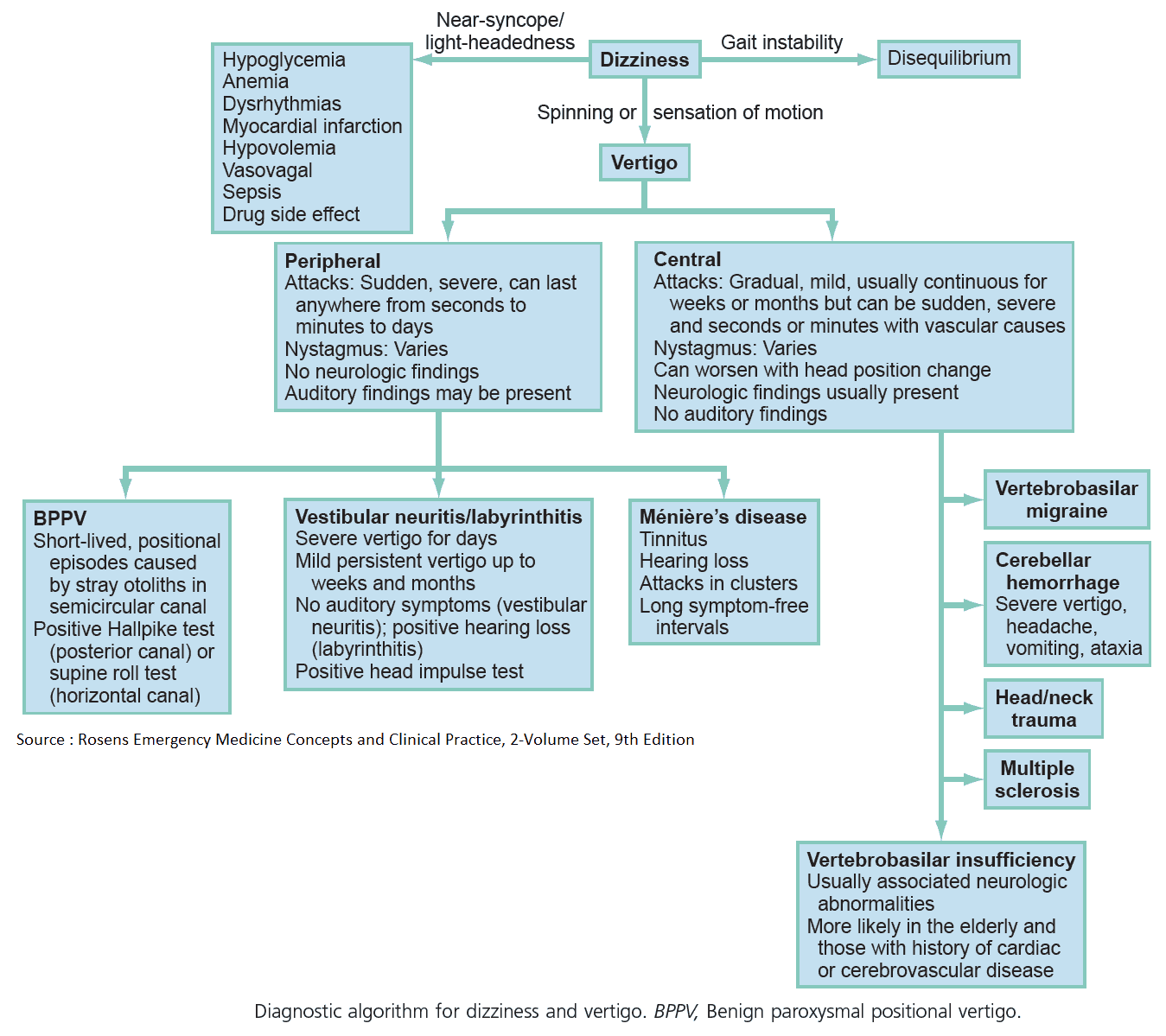
True vertigo is the false perception (illusion) of movement, usually rotational, of a patient of his or her surroundings. This is often accompanied by vomiting, sweating, and pallor.
It results from disease in the labyrinth (most common cause), the 8th cranial nerve, or its connections in the brainstem.
Dizziness (i.e., presyncope) or Unsteadiness
Dizziness (i.e., presyncope) or unsteadiness without vertigo can result from a variety of unrelated disorders. Patients often complain of feeling as if they are going to “pass out.” They may say that their vision became yellow or that they “saw stars.” They do not complain of things spinning. These are discussed in more detail in their appropriate chapters.
Dizziness may also be accompanied by sweating and nausea and may be tied to specific movements (i.e., moving from seated to standing). Disorders causing dizziness are discussed in more detail in their appropriate chapters.
When a patient presents with “vertigo” or “dizziness,” it is vital to establish whether true vertigo is present or not, as these symptoms result from different pathologies.
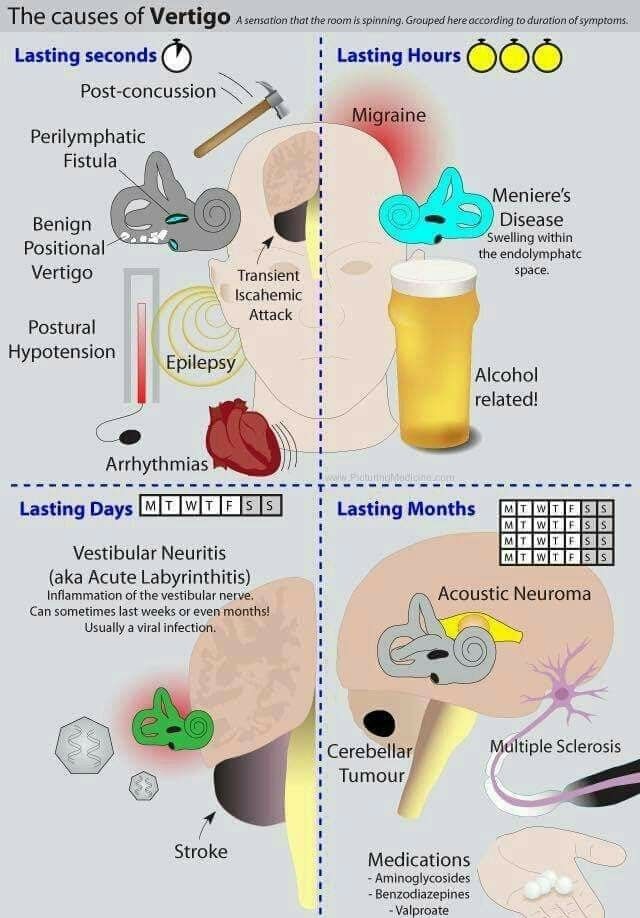
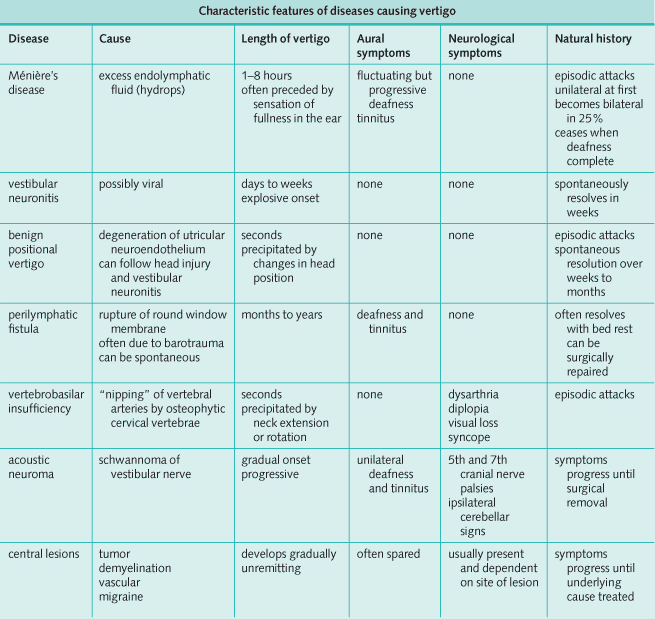
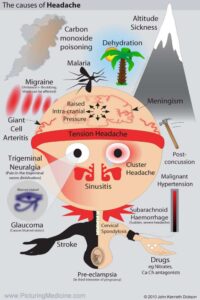
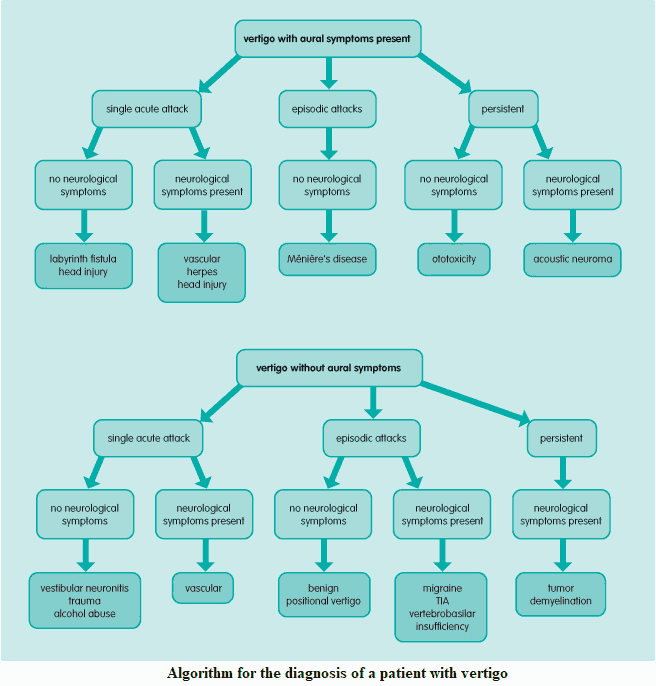
Differential Diagnosis of Vertigo
1. Labyrinth disorders
- Middle ear disease (e.g., otitis media).
- Ménière’s disease (triad of vertigo, tinnitus, and sensorineural hearing loss).
- Benign positional vertigo: most commonly caused by free calcium debris within the posterior semicircular canal (canalithiasis).
- Labyrinthitis.
- Traumatic vertigo.
- Perilymphatic fistula.
- Syphilitic labyrinthitis.
2. 8th cranial nerve disease
- Vestibular neuronitis.
- Acoustic neuroma.
- Ramsay Hunt syndrome: herpes zoster of the geniculate ganglion.
- Ototoxic drugs: aminoglycosides such as gentamicin.
3. Brainstem lesions
- Multiple sclerosis: demyelination.
- Vertebrobasilar ischemia: transient ischemic attack.
- Stroke: lateral medullary syndrome (infraction of interior cerebellar artery).
- Vertebrobasilar insufficiency.
- Migraine.
- Encephalitis.
- Tumor.
- Syringobulbia.
- Alcohol abuse.
Note that vertigo may also be a feature of temporal lobe pathology.
Differential Diagnosis of Dizziness
- Low cardiac output.
- Hyperventilation, anxiety.
- Psychiatric disturbance-panic attack.
- Anemia.
- Hypoglycemia.
- Pheochromocytoma.
- Postural hypotension due to drugs (e.g., overenthusiastic antihypertensive regimens, antidepressants, tranquilizers).
- Visual disturbance.
- Cerebrovascular disease.
- Fever.
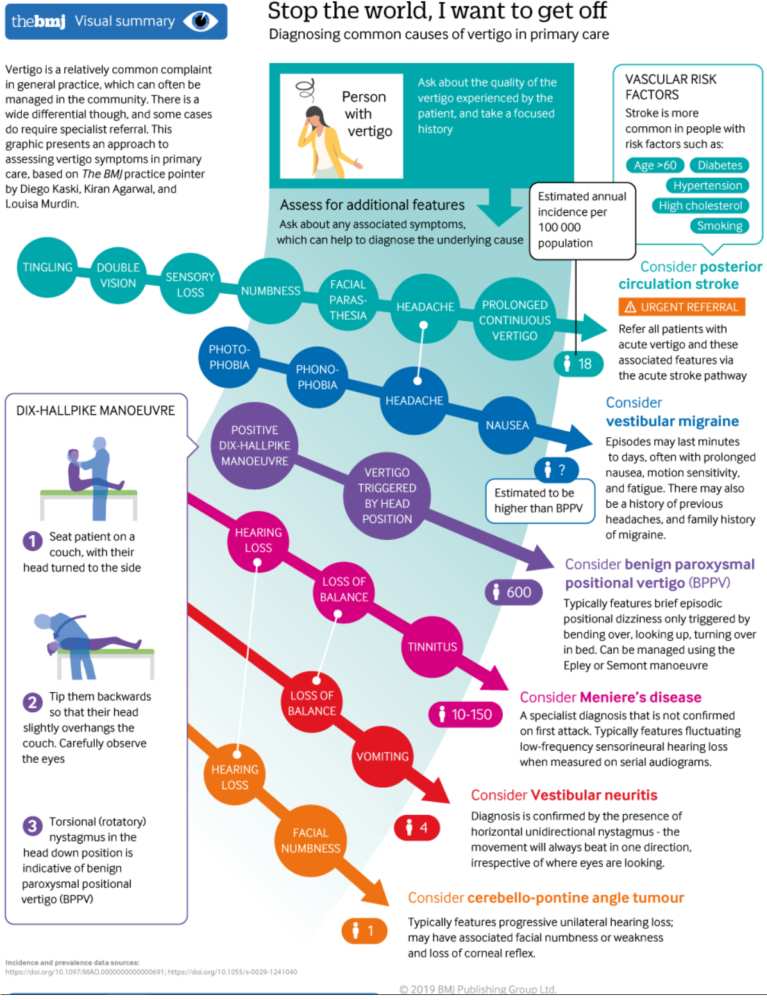
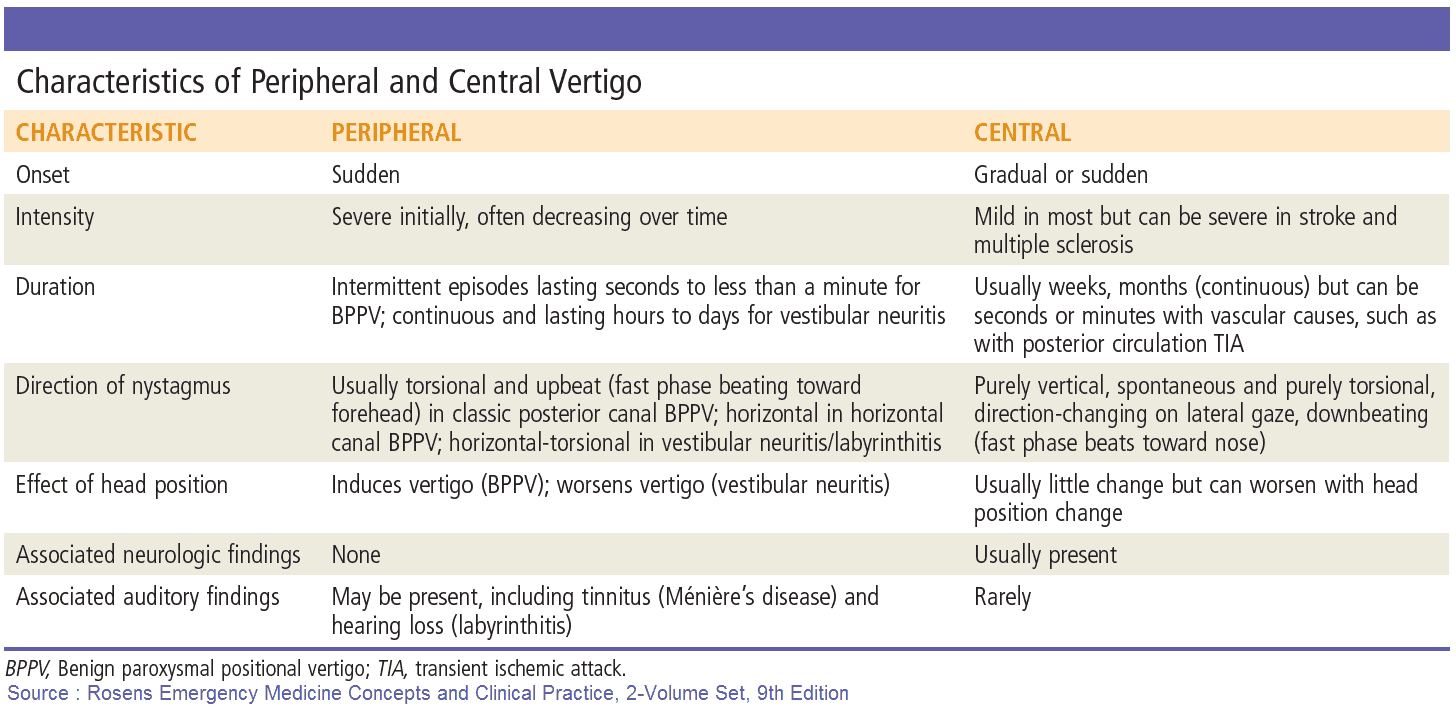
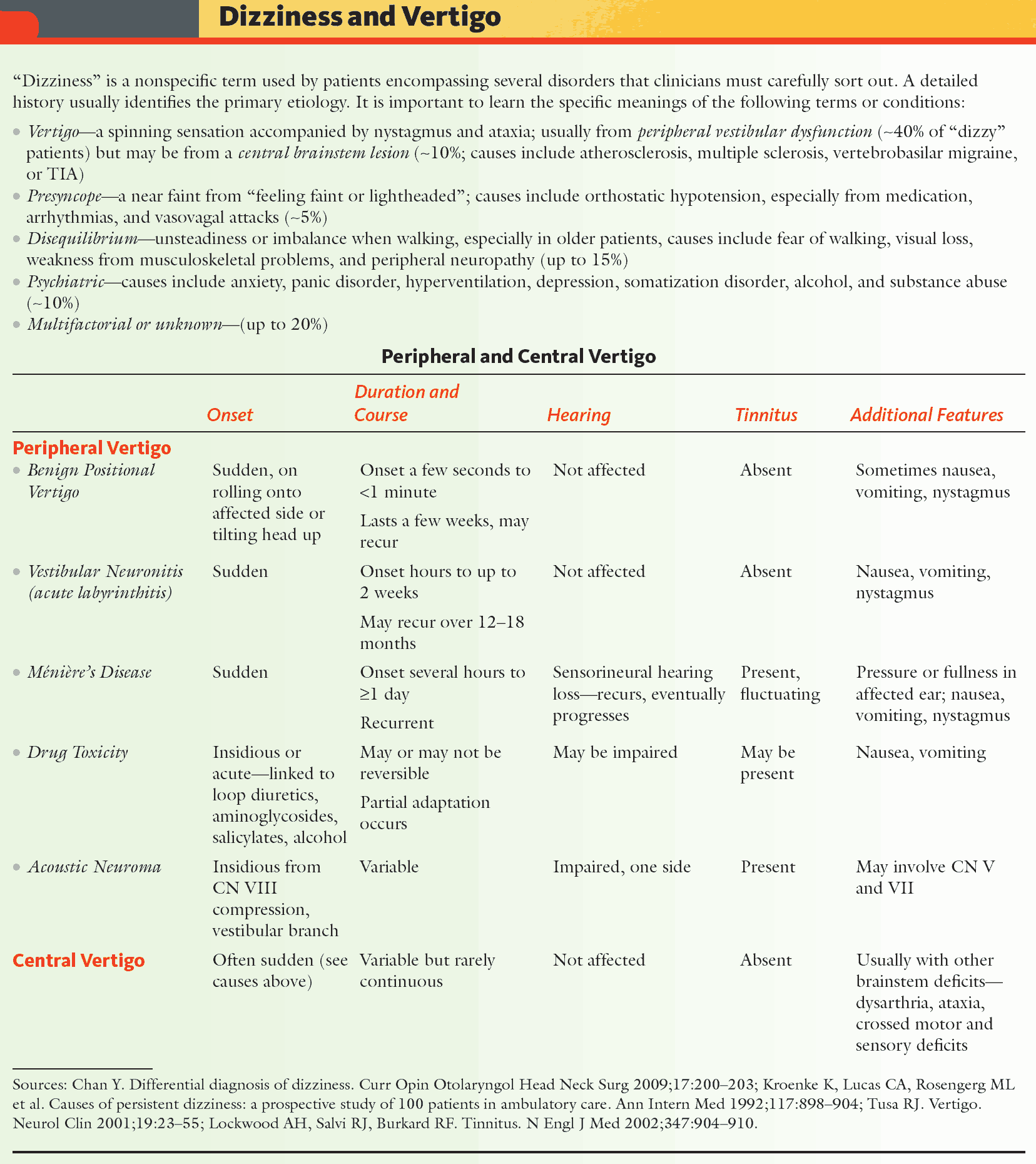
Symptoms and History in the Patient with Vertigo
The diagnosis in patients with vertigo is largely made on the history. It is important to elicit the time course of the vertigo and the likely site of the lesion by asking about other auditory and neurological symptoms.
Pattern of vertigo
The following should be established:
- Onset: peripheral lesions generally cause acute severe symptoms; central lesions tend to cause a gradual onset with less severe vertigo. Peripheral lesions also tend to cause nystagmus with a rotary component, whereas central lesions cause nystagmus that lacks rotary movement and is vertical in nature.
- Duration of vertigo.
- Recurrent episodes or a single attack?
- Relation to head position.
- Associated symptoms: dyspnea, tachycardia, and anxiety suggest a panic attack.
Aural symptoms
The presence of aural symptoms suggests that the lesion is peripheral, involving the labyrinth or 8th cranial nerve:
- Ear pain.
- Ear discharge.
- Deafness (fluctuating or progressive).
- Tinnitus (ringing in the ear[s]).
Neurologic symptoms
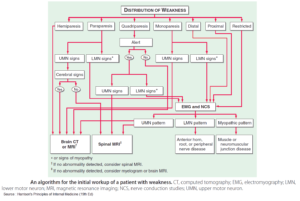
The following symptoms suggest central pathology or acoustic neuroma.
- Facial weakness.
- Dysarthria.
- Dysphagia.
- Diplopia.
- Loss of consciousness.
- Seizures.
- Weakness, altered sensation, poor limb coordination.
History suggestive of an underlying cause
- Recent viral illness causes vestibular neuronitis.
- Previous head injury may lead to labyrinth concussion, benign positional vertigo.
- Previous otologic surgery.
- Drug history (e.g., aminoglycosides).
- Risk factors for vascular disease: hypertension, high cholesterol, smoking, family history.
- Recent flying or diving (e.g., barotrauma-perilymphatic fistula).
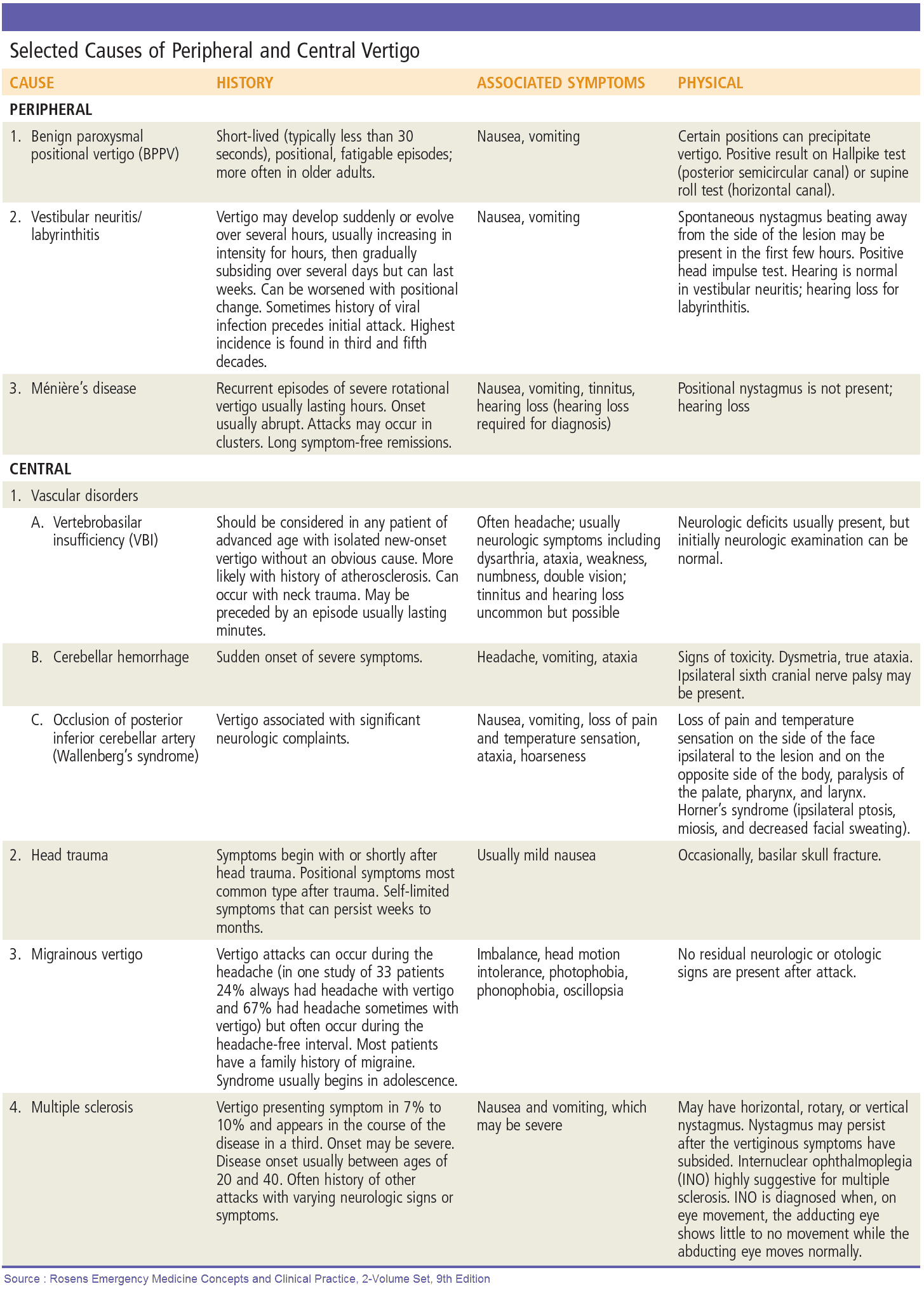
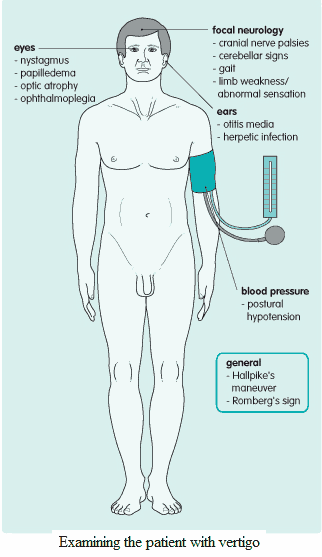
Examination and Signs in the Patient with Vertigo
The clinical examination is often normal. The following specific abnormalities should be looked for carefully:
- Nystagmus: horizontal and away (fast phase) from the side of the lesion. Occasionally, brainstem lesions may also cause vertical nystagmus. Direction of nystagmus is as noted above.
- Romberg’s sign: positive if the patient is more unsteady on standing when the eyes are closed compared with when they are open; in vestibular disorders. The patient will tend to fall to the side of the lesion.
- Hallpike’s maneuver: the patient is asked to lie down quickly with the head tilted to one side; in benign positional vertigo there will be a latent period of a few seconds followed by nystagmus.
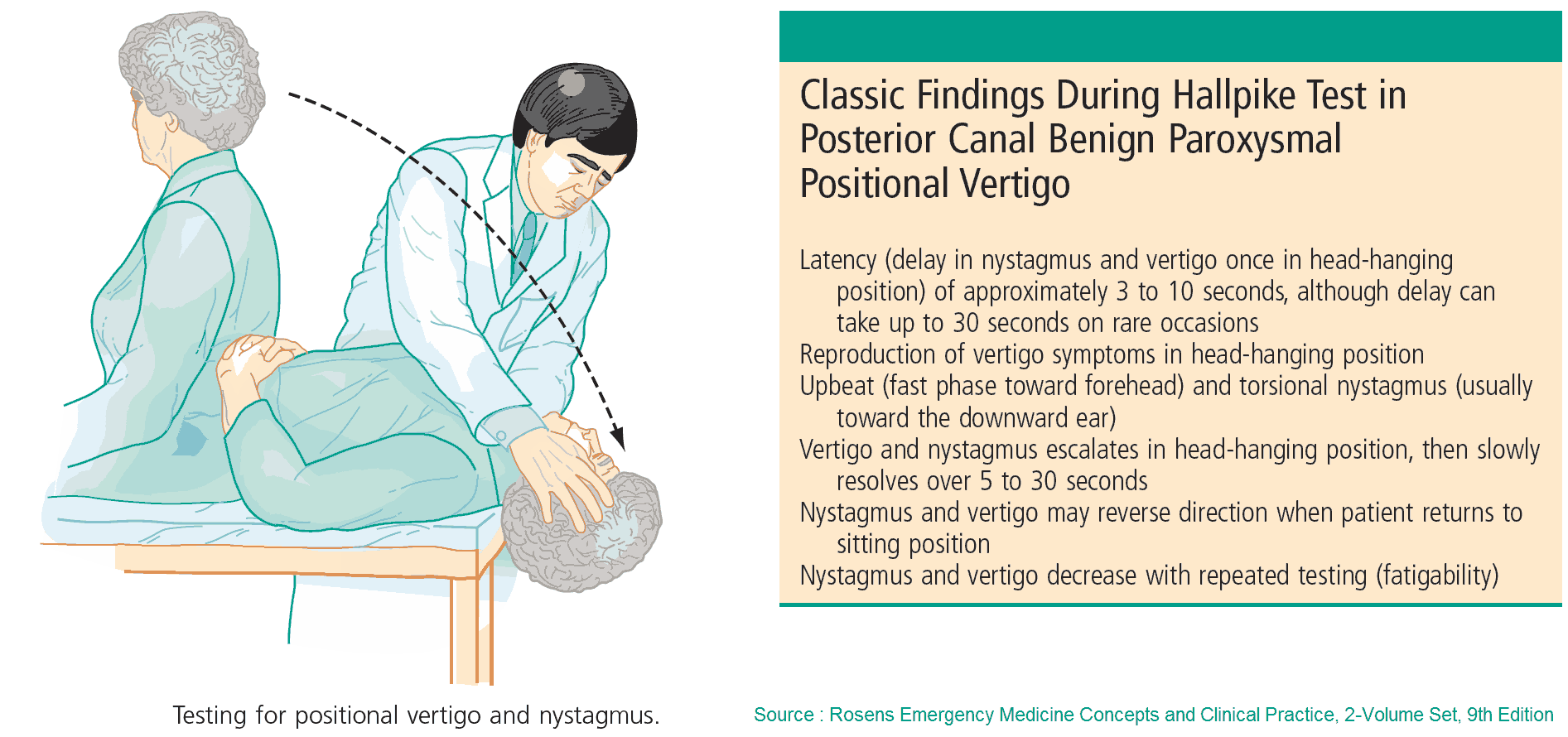
- Focal neurologic signs: if present, these suggest a central lesion, acoustic neuroma, or Ramsay Hunt syndrome. Pay particular attention to assessment of the 8th cranial nerve, gait, and cerebellar signs.
- Eyes: papilledema (tumor with raised intracranial pressure), optic atrophy (demyelination), and ophthalmoplegia (cranial nerve defect, demyelination).
- Ears: otoscopy may reveal otitis media or a herpetic rash. Herpetic lesions may also be found on careful examination of the surrounding skin. Lying and standing blood pressures: postural hypotension.
Investigating and Diagnosing the Patient with Vertigo
- Audiometry: to distinguish between conductive and sensorineural deafness.
- Caloric tests: normally, running cold and then warm water into the external auditory meatus causes contralateral and then ipsilateral nystagmus, respectively; where there is pathology in the ipsilateral labyrinth, 8th cranial nerve, or brainstem, this normal response will be reduced or absent.
- Electronystagmography: a more accurate assessment of the presence and type of nystagmus.
- Imaging: high-resolution computed tomography scanning and magnetic resonance imaging are useful tools when a central lesion or acoustic neuroma is suspected.
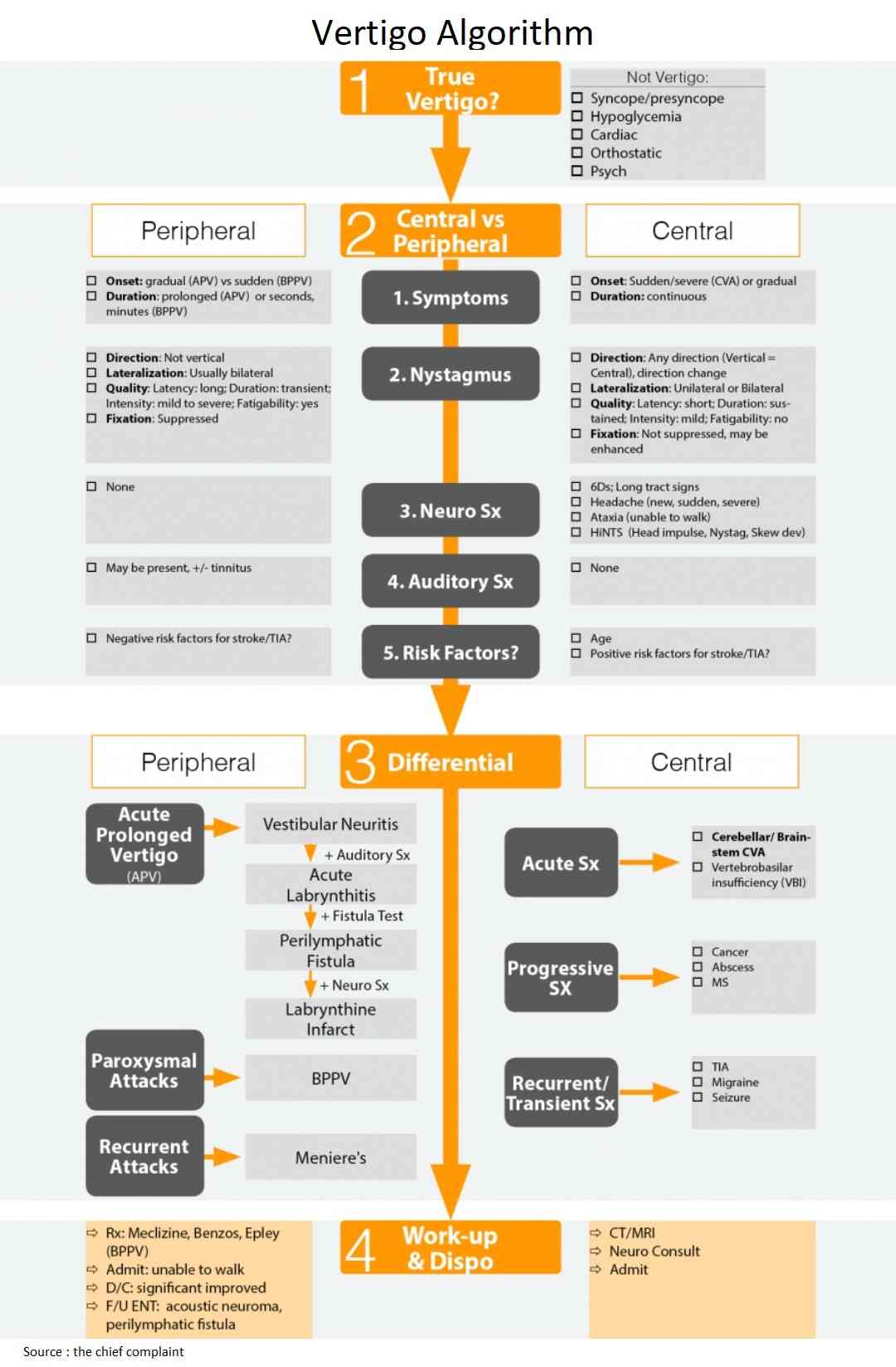
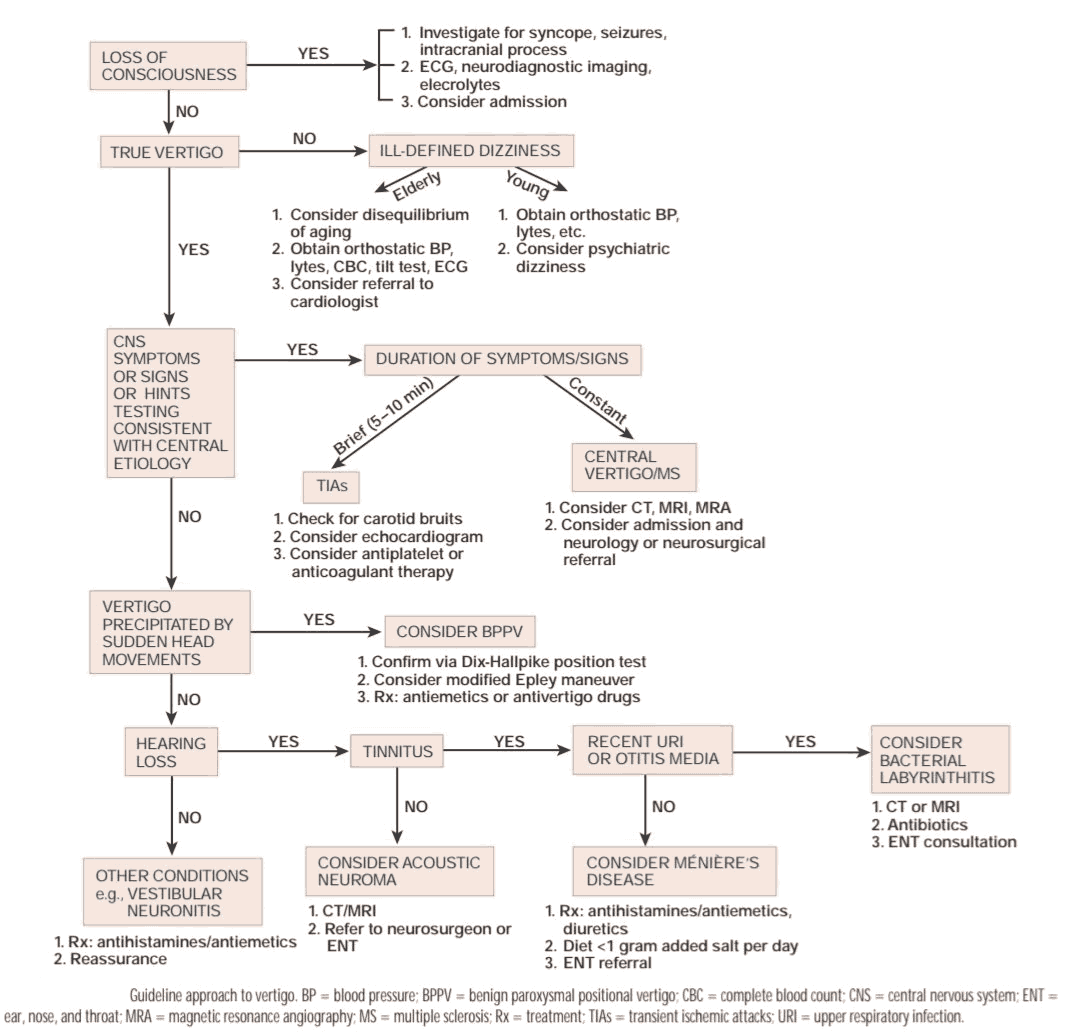
READ MORE about : Vertigo Algorithm and Differential Diagnosis