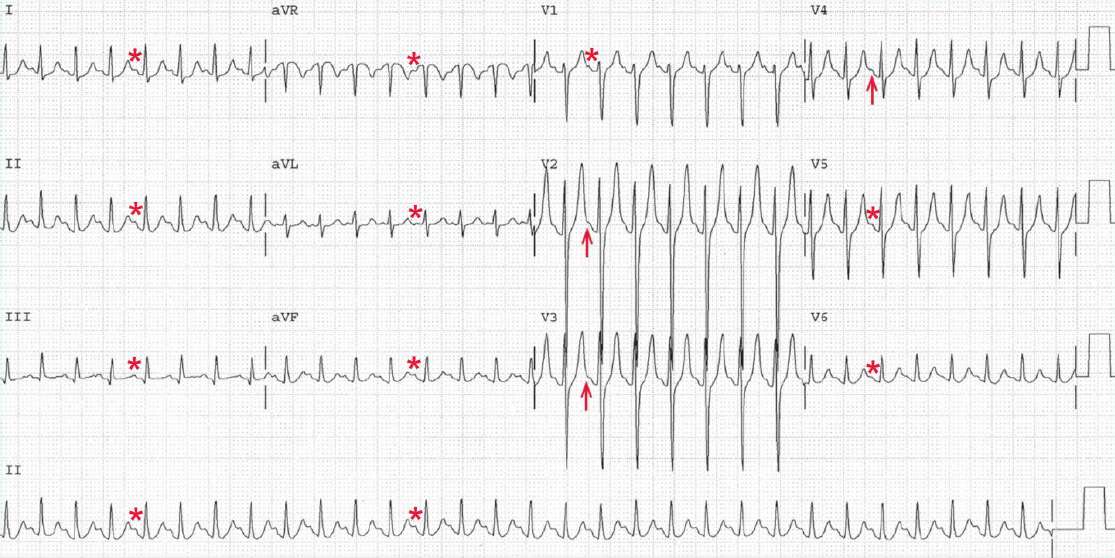
There is a regular rhythm at a rate of 180 bpm. Although not obvious in every lead, a P wave (*) can be seen before each QRS complex, particularly in leads I, II, III, and aVF.
In the precordial leads, P waves (arrow) can be seen at the very end of the T waves. The PR interval is constant (0.12 sec). The P waves are positive in leads I, II, aVF, and V4-V6. Therefore, this is sinus tachycardia.
In the presence of sinus tachycardia, the P waves are often superimposed on the T waves, especially if the PR interval is prolonged. Hence it is important to look carefully at the T waves when P waves are not readily apparent.
It should be noted that T waves should be smooth in upstroke and downstroke. Notching or bumps on T waves are very suggestive of superimposed P waves.
The QRS complex duration (0.08 sec) and morphology are normal. The QRS axis in the frontal plane is normal, between 0° and +90° (positive QRS complex in leads I and aVF). The QT/QTc intervals are normal (240/400 msec).
The PR interval is short, based on the definition of a normal PR interval (between 0.14 and 0.20 sec). However, the PR interval does change with heart rate as a result of changes in sympathetic and parasympathetic inputs into the AV node.
Sinus tachycardia is generally the result of increased sympathetic activity, which causes an increase in conduction velocity through the AV node. Therefore, sinus tachycardia is associated with a shortening of the PR interval.
In contrast, sinus bradycardia, which is due to withdrawal of sympathetic stimulation and increased parasympathetic activity, is associated with a decreased conduction velocity through the AV node and hence an increase in the PR interval.
Sinus tachycardia is usually the result of sympathetic activation or an increase in circulating catecholamines. There are many possible etiologies for sinus tachycardia with hypotension, including any severe infection with or without sepsis, pulmonary embolism, adrenal insufficiency, acute bleeding or hypovolemia, and cardiogenic shock.