Table of Contents
Summary of Pharmacological Therapies for ME/CFS, Long Covid and Fibromyalgia
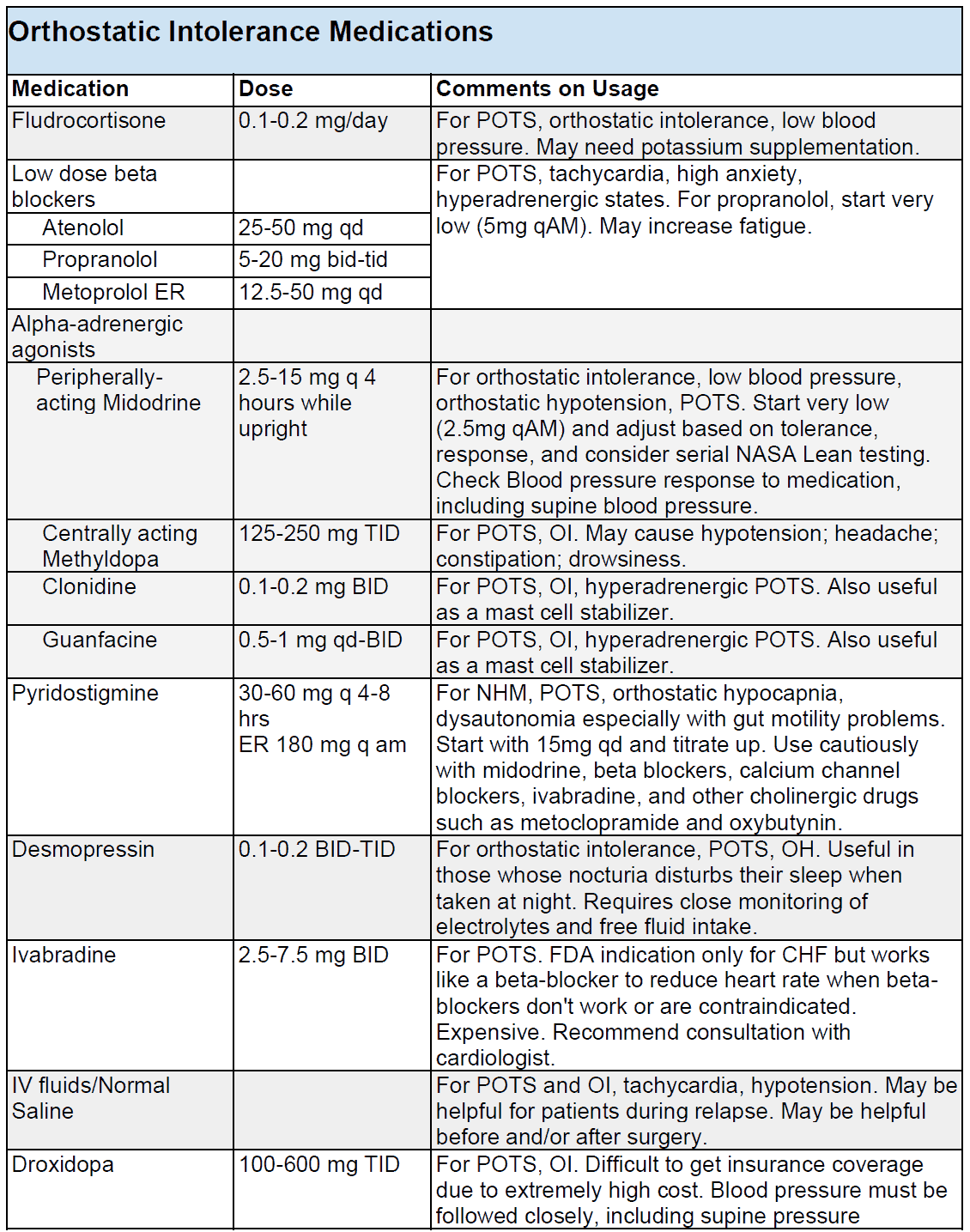
1. POTS, Dysautonomia and Orthostatic Intolerance Medications/Drugs
- Fludrocortisone 0.1-0.2 mg/day
- For POTS, orthostatic intolerance, low blood pressure. May need potassium supplementation.
- Low Dose Beta Blockers – For POTS, tachycardia, high anxiety, hyperadrenergic states. May increase fatigue.
- Atenolol 25-50 mg once a day
- Propranolol 5-20 mg twice or three times a day (start very low (5mg in the morning))
- Metoprolol ER 12.5-50 mg once a day
- Alpha-adrenergic Agonists
- Peripherally- acting Midodrine 2.5-15 mg q 4 hours while upright
- For orthostatic intolerance, low blood pressure, orthostatic hypotension, POTS. Start very low (2.5mg every morning) and adjust based on tolerance, response, and consider serial NASA Lean testing. Check Blood pressure response to medication, including supine blood pressure.
- Centrally acting Methyldopa 125-250 mg three times a day
- For POTS, OI. May cause hypotension; headache; constipation; drowsiness.
- Clonidine 0.1-0.2 mg twice a day
- For POTS, OI, hyperadrenergic POTS. Also useful as a mast cell stabilizer.
- Guanfacine 0.5-1 mg once or twice a day
- For POTS, OI, hyperadrenergic POTS. Also useful as a mast cell stabilizer.
- Peripherally- acting Midodrine 2.5-15 mg q 4 hours while upright
- Pyridostigmine 30-60 mg every 4-8 hrs (Extended Release 180 mg every morning
- For NHM, POTS, orthostatic hypocapnia, dysautonomia especially with gut motility problems. Start with 15mg once a day and titrate up. Use cautiously with midodrine, beta blockers, calcium channel blockers, ivabradine, and other cholinergic drugs such as metoclopramide and oxybutynin.
- Desmopressin 0.1-0.2 twice or three times a day
- For orthostatic intolerance, POTS, OH. Useful in those whose nocturia disturbs their sleep when taken at night. Requires close monitoring of electrolytes and free fluid intake.
- Ivabradine 2.5-7.5 mg twice a day
- For POTS. FDA indication only for CHF but works like a beta-blocker to reduce heart rate when beta-blockers don’t work or are contraindicated. Expensive. Recommend consultation with cardiologist.
- IV fluids/Normal Saline
- For POTS and OI, tachycardia, hypotension. May be helpful for patients during relapse. May be helpful before and/or after surgery.
- Droxidopa 100-600 mg three times a day
- For POTS, OI. Difficult to get insurance coverage due to extremely high cost. Blood pressure must be followed closely, including supine pressure
Abbreviations:
OI: Orthostatic intolerance
POTS: postural orthostatic tachycardia syndrome
NMH: neurally mediated hypotension
CHF: chronic heart failure
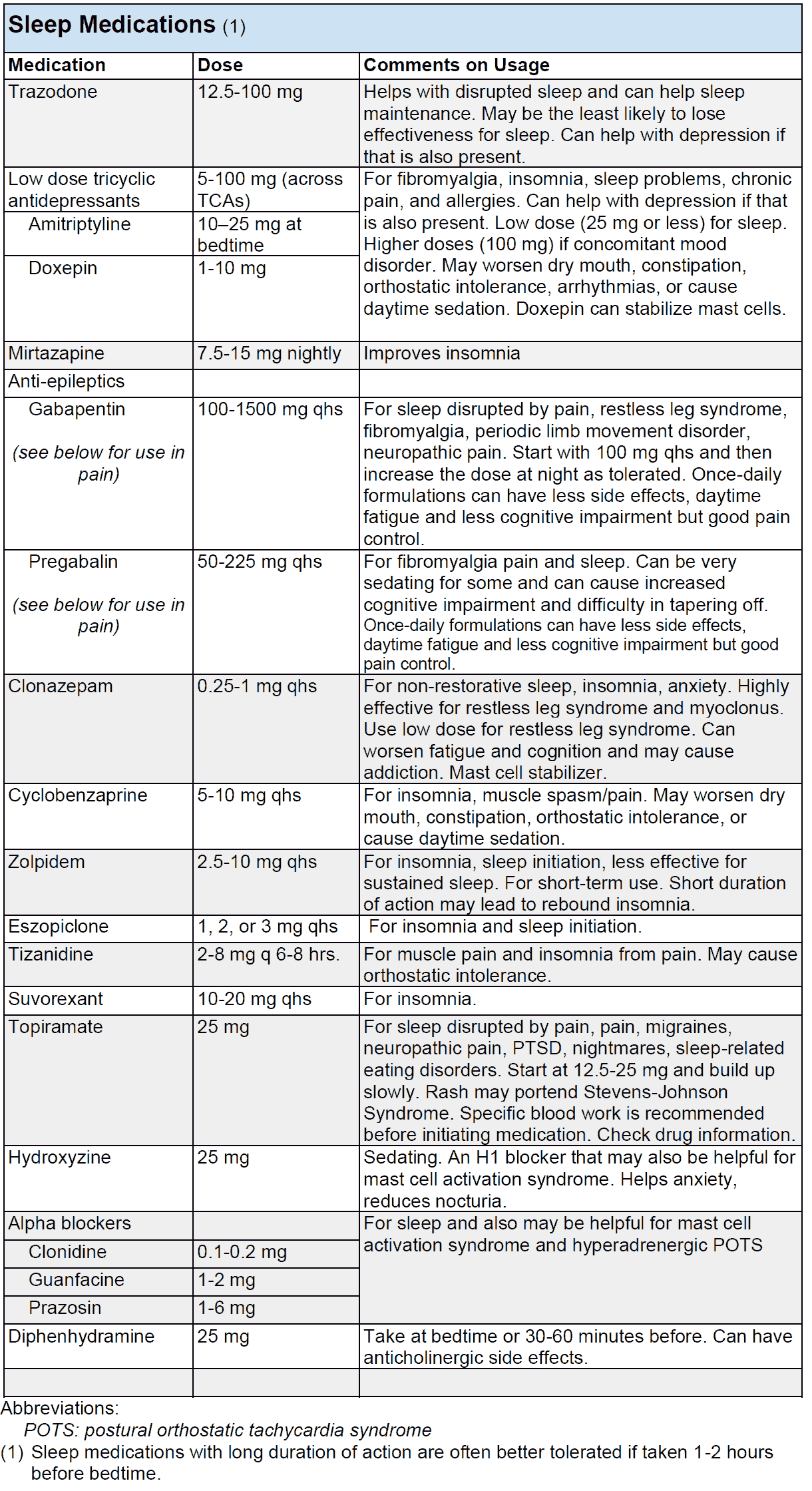
2. Sleep Medications/Drugs Used in ME/CFS, Long Covid and Fibromyalgia
- Trazodone 12.5-100 mg
- Helps with disrupted sleep and can help sleep maintenance. May be the least likely to lose effectiveness for sleep. Can help with depression if that is also present.
- Low dose tricyclic antidepressants (TCA) 5-100 mg (across TCAs) – For fibromyalgia, insomnia, sleep problems, chronic pain, and allergies. Can help with depression if that is also present. Low dose (25 mg or less) for sleep. Higher doses (100 mg) if concomitant mood disorder. May worsen dry mouth, constipation, orthostatic intolerance, arrhythmias, or cause daytime sedation. Doxepin can stabilize mast cells.
- Amitriptyline 10–25 mg at bedtime
- Doxepin 1-10 mg (can stabilize mast cells)
- Mirtazapine 7.5-15 mg nightly
- Improves insomnia
- Anti-epileptics
- Gabapentin (see below for use in pain) 100-1500 mg at bedtime
- For sleep disrupted by pain, restless leg syndrome, fibromyalgia, periodic limb movement disorder, neuropathic pain. Start with 100 mg qhs and then increase the dose at night as tolerated. Once-daily formulations can have less side effects, daytime fatigue and less cognitive impairment but good pain control.
- Pregabalin (see below for use in pain) 50-225 mg at bedtime
- For fibromyalgia pain and sleep. Can be very sedating for some and can cause increased cognitive impairment and difficulty in tapering off. Once-daily formulations can have less side effects, daytime fatigue and less cognitive impairment but good pain control.
- Gabapentin (see below for use in pain) 100-1500 mg at bedtime
- Clonazepam 0.25-1 mg at bedtime.
- For non-restorative sleep, insomnia, anxiety. Highly effective for restless leg syndrome and myoclonus. Use low dose for restless leg syndrome. Can worsen fatigue and cognition and may cause addiction. Mast cell stabilizer.
- Cyclobenzaprine 5-10 mg at bedtime.
- For insomnia, muscle spasm/pain. May worsen dry mouth, constipation, orthostatic intolerance, or cause daytime sedation.
- Zolpidem 2.5-10 mg at bedtime.
- For insomnia, sleep initiation, less effective for sustained sleep. For short-term use. Short duration of action may lead to rebound insomnia.
- Eszopiclone 1, 2, or 3 mg at bedtime
- For insomnia and sleep initiation.
- Tizanidine 2-8 mg every 6-8 hrs.
- For muscle pain and insomnia from pain. May cause orthostatic intolerance.
- Suvorexant 10-20 mg at bedtime
- For insomnia.
- Topiramate 25 mg
- For sleep disrupted by pain, pain, migraines, neuropathic pain, PTSD, nightmares, sleep-related eating disorders. Start at 12.5-25 mg and build up slowly. Rash may portend Stevens-Johnson Syndrome. Specific blood work is recommended before initiating medication. Check drug information.
- Hydroxyzine 25 mg
- Sedating. An H1 blocker that may also be helpful for mast cell activation syndrome. Helps anxiety, reduces nocturia.
- Alpha blockers – For sleep and also may be helpful for mast cell activation syndrome and hyperadrenergic POTS
- Clonidine 0.1-0.2 mg
- Guanfacine 1-2 mg
- Prazosin 1-6 mg
- Diphenhydramine 25 mg
- Take at bedtime or 30-60 minutes before. Can have anticholinergic side effects.
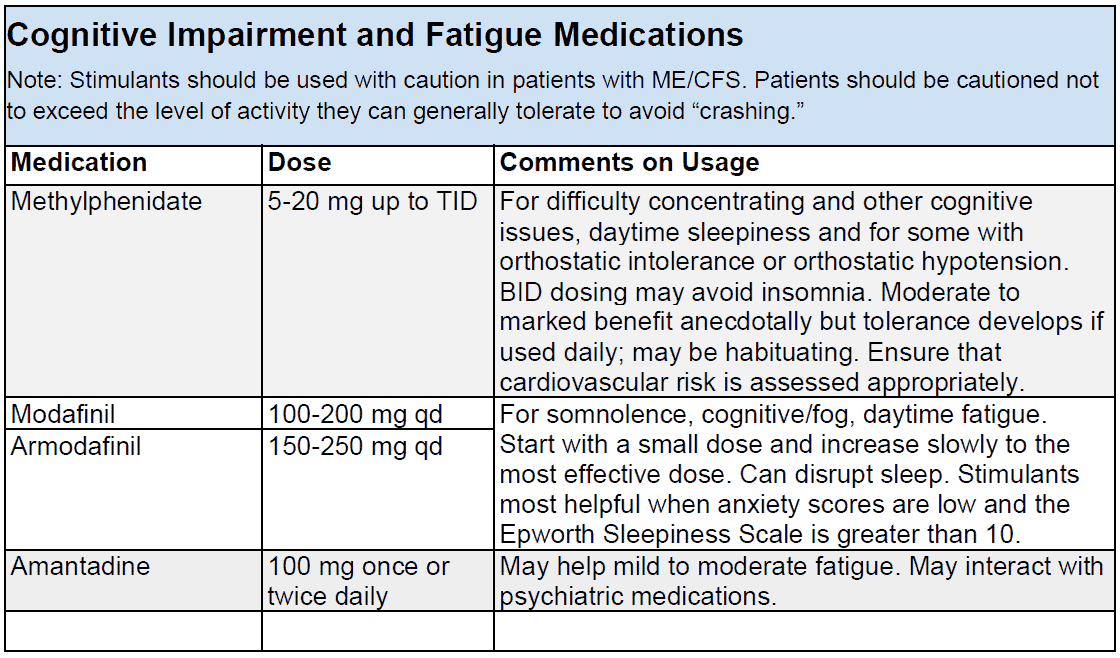
3. Cognitive Impairment and Fatigue Medications/Drugs
- Methylphenidate 5-20 mg up to three time a day.
- For difficulty concentrating and other cognitive issues, daytime sleepiness and for some with orthostatic intolerance or orthostatic hypotension. BID dosing may avoid insomnia. Moderate to marked benefit anecdotally but tolerance develops if used daily; may be habituating. Ensure that cardiovascular risk is assessed appropriately.
- Modafinil 100-200 mg once a day OR Armodafinil 150-250 mg once a day.
- For somnolence, cognitive/fog, daytime fatigue. Start with a small dose and increase slowly to the most effective dose. Can disrupt sleep. Stimulants most helpful when anxiety scores are low and the Epworth Sleepiness Scale is greater than 10.
- Amantadine 100 mg once or twice daily
- May help mild to moderate fatigue. May interact with psychiatric medications.
- Low Dose Atypical Antipsychotics – For fatigue, PEM, cognitive impairment, sensory hypersensitivity.
- Low Dose Aripirazole (Abilify) (LDA) 0.1-2 mg once a day (start with smallest dose and slowly increase by 0.1-0.2mg every week or two.
- Low Dose Sulpiride 50-100 mg once a day
- Low Dose Amisulpride 25-50mg once a day
- Nicotine Patches 7-14 mg 24/hour patch for 14 to 30 days.
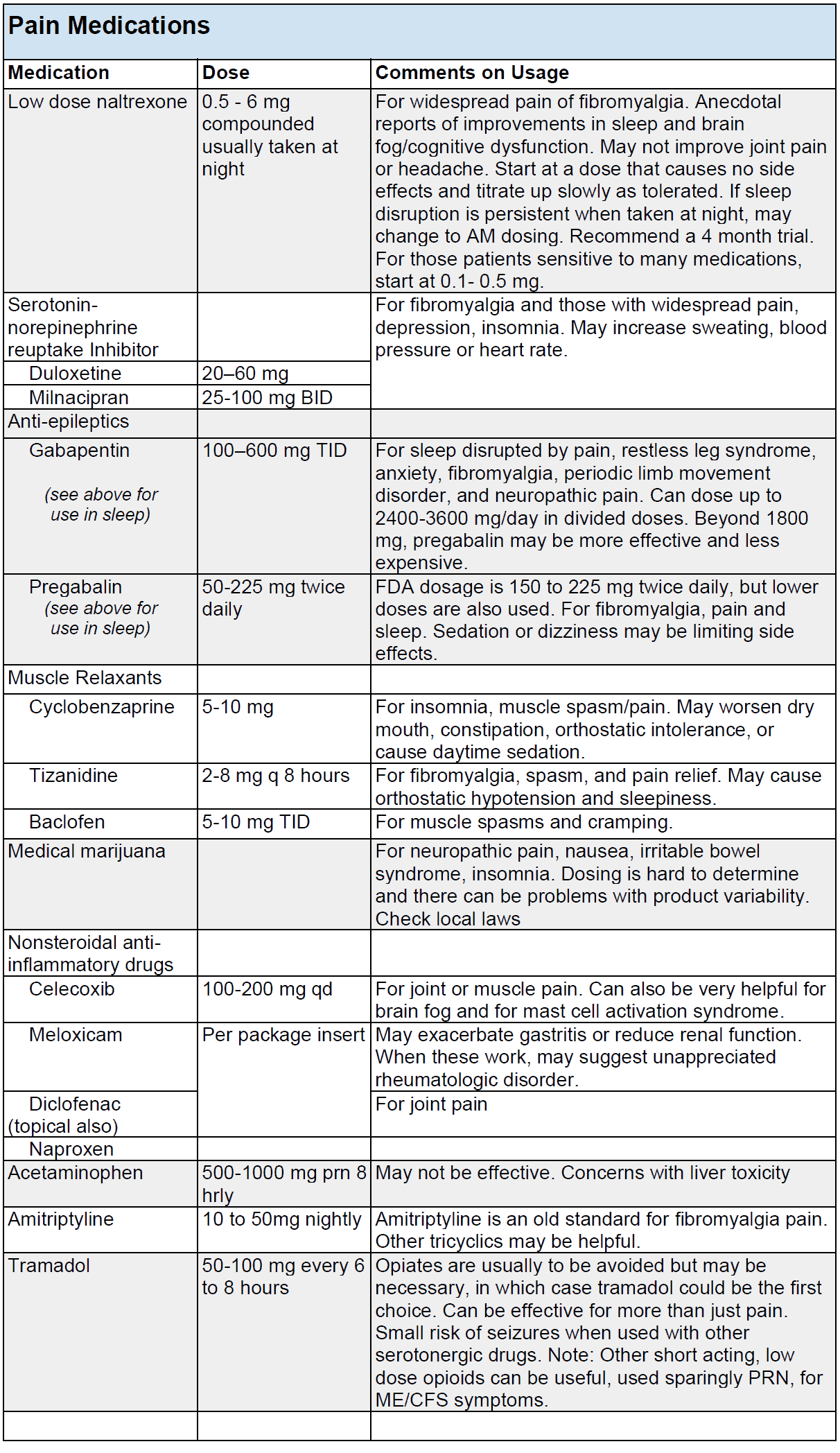
4. Pain Medications/Drugs used in ME/CFS, Long Covid and Fibromyalgia
- Low Dose Naltrexone 0.5 – 6 mg compounded usually taken at night
- For widespread pain of fibromyalgia. Anecdotal reports of improvements in sleep and brain fog/cognitive dysfunction. May not improve joint pain or headache. Start at a dose that causes no side effects and titrate up slowly as tolerated. If sleep disruption is persistent when taken at night, may change to AM dosing. Recommend a 4 month trial. For those patients sensitive to many medications, start at 0.1- 0.5 mg.
- Serotonin-Norepinephrine Reuptake Inhibitor (SNRI) – For fibromyalgia and those with widespread pain, depression, insomnia. May increase sweating, blood pressure or heart rate.
- Duloxetine 20–60 mg
- Milnacipran 25-100 mg twice a day
- Anti-epileptics
- Gabapentin (see above for use in sleep) 100–600 mg three time a day
- For sleep disrupted by pain, restless leg syndrome, anxiety, fibromyalgia, periodic limb movement disorder, and neuropathic pain. Can dose up to 2400-3600 mg/day in divided doses. Beyond 1800 mg, pregabalin may be more effective and less expensive.
- Pregabalin (see above for use in sleep) 50-225 mg twice daily
- FDA dosage is 150 to 225 mg twice daily, but lower doses are also used. For fibromyalgia, pain and sleep. Sedation or dizziness may be limiting side effects.
- Gabapentin (see above for use in sleep) 100–600 mg three time a day
- Muscle Relaxants
- Cyclobenzaprine 5-10 mg
- For insomnia, muscle spasm/pain. May worsen dry mouth, constipation, orthostatic intolerance, or cause daytime sedation.
- Tizanidine 2-8 mg every 8 hours
- For fibromyalgia, spasm, and pain relief. May cause orthostatic hypotension and sleepiness.
- Baclofen 5-10 mg three time a day
- For muscle spasms and cramping.
- Cyclobenzaprine 5-10 mg
- Medical marijuana
- For neuropathic pain, nausea, irritable bowel syndrome, insomnia. Dosing is hard to determine and there can be problems with product variability. Check local laws.
- Nonsteroidal anti-inflammatory drugs
- Celecoxib 100-200 mg once a day
- For joint or muscle pain. Can also be very helpful for brain fog and for mast cell activation syndrome.
- Meloxicam
- May exacerbate gastritis or reduce renal function. When these work, may suggest unappreciated rheumatologic disorder.
- Diclofenac (topical also)
- For joint pain
- Celecoxib 100-200 mg once a day
- Acetaminophen 500-1000 mg as needed every 8 hours
- May not be effective. Concerns with liver toxicity.
- Amitriptyline 10 to 50mg nightly
- Amitriptyline is an old standard for fibromyalgia pain. Other tricyclics may be helpful.
- Tramadol 50-100 mg every 6 to 8 hours
- Opiates are usually to be avoided but may be necessary, in which case tramadol could be the first choice. Can be effective for more than just pain. Small risk of seizures when used with other serotonergic drugs. Note: Other short acting, low dose opioids can be useful, used sparingly as needed, for ME/CFS symptoms.
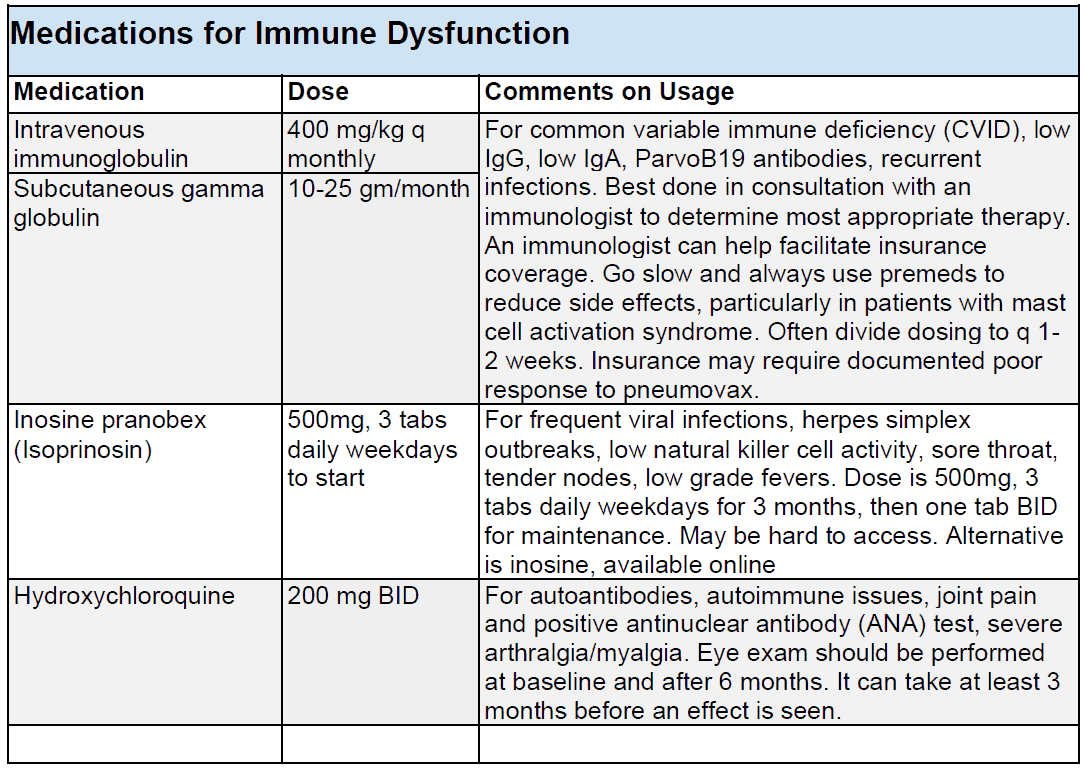
5. Medications/Drugs for Immune Dysfunction and Autoimmunity in ME/CFS, Long Covid and Fibromyalgia
- Intravenous immunoglobulin 400 mg/kg q monthly OR Subcutaneous gamma globulin 10-25 gm/month
- For common variable immune deficiency (CVID), low IgG, low IgA, ParvoB19 antibodies, recurrent infections. Best done in consultation with an immunologist to determine most appropriate therapy. An immunologist can help facilitate insurance coverage. Go slow and always use premeds to reduce side effects, particularly in patients with mast cell activation syndrome. Often divide dosing to q 1-2 weeks. Insurance may require documented poor response to pneumovax.
- Inosine pranobex (Isoprinosin) 500mg, 3 tabs daily weekdays to start
- For frequent viral infections, herpes simplex outbreaks, low natural killer cell activity, sore throat, tender nodes, low grade fevers. Dose is 500mg, 3 tabs daily weekdays for 3 months, then one tab twice a day for maintenance. May be hard to access. Alternative is inosine, available online .
- Hydroxychloroquine 200 mg twice a day
- For autoantibodies, autoimmune issues, joint pain and positive antinuclear antibody (ANA) test, severe arthralgia/myalgia. Eye exam should be performed at baseline and after 6 months. It can take at least 3 months before an effect is seen.
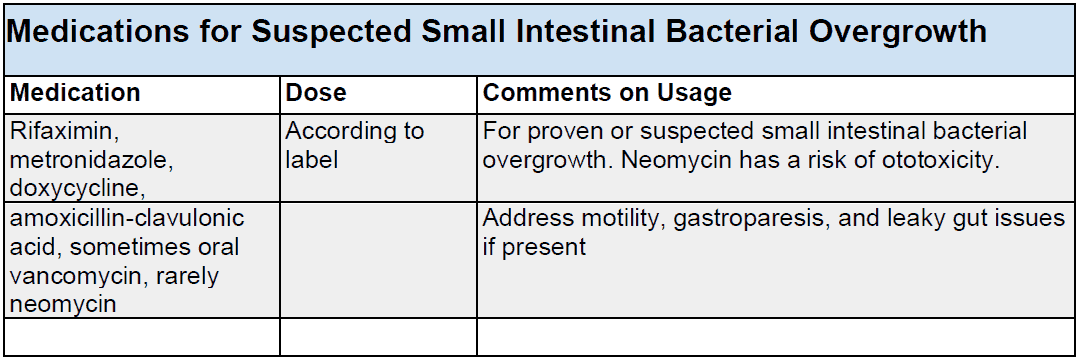
6. Medications/Drugs for Suspected Small Intestinal Bacterial Overgrowth (SIBO) in ME/CFS and Long Covid
- Rifaximin, metronidazole, doxycycline
- For proven or suspected small intestinal bacterial overgrowth. Neomycin has a risk of ototoxicity.
- Amoxicillin-clavulonic acid, sometimes oral vancomycin, rarely neomycin
- Address motility, gastroparesis, and leaky gut issues if present
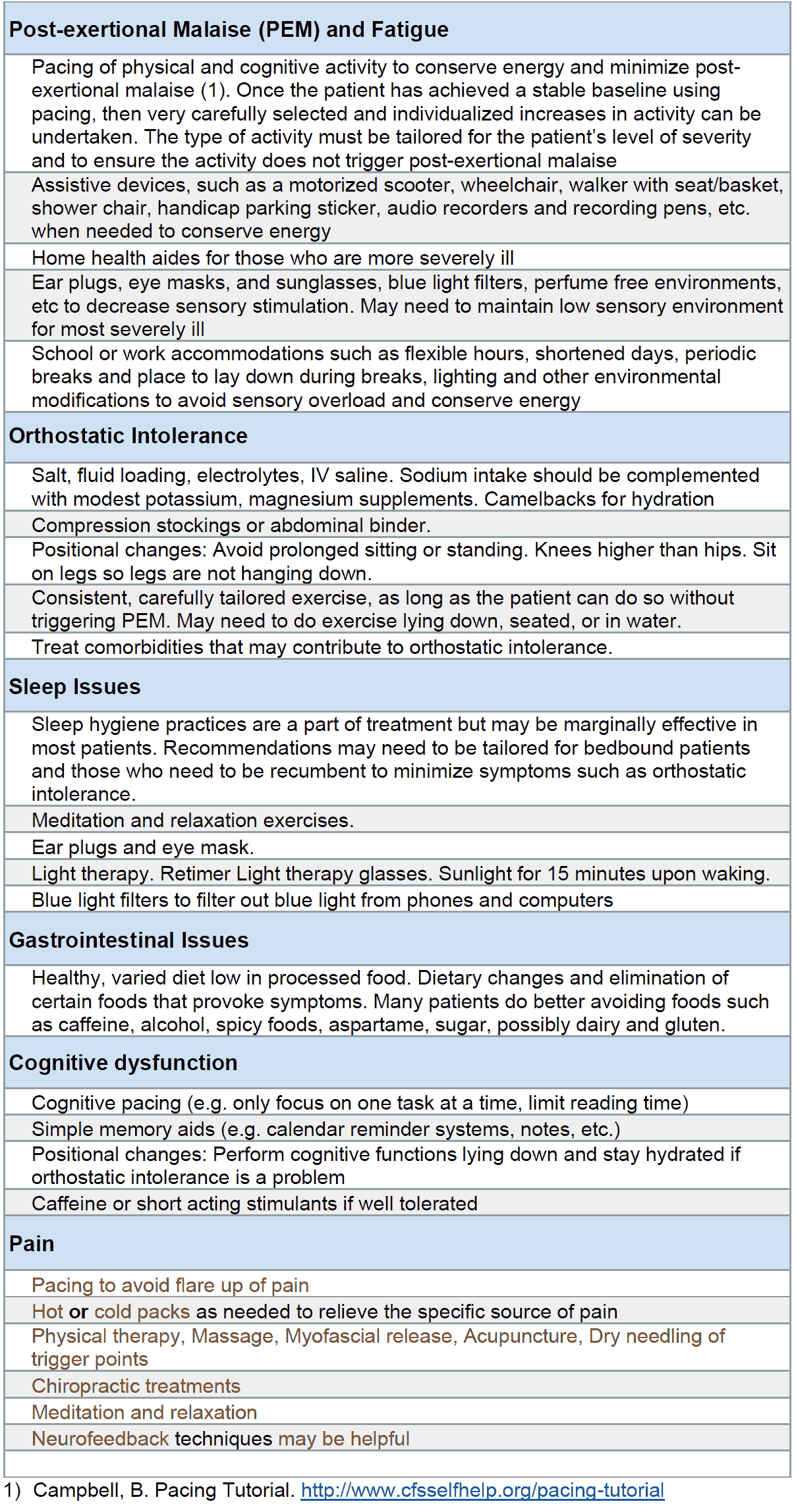
Summary of Non-Pharmacological Therapies for ME/CFS, Long Covid and Fibromyalgia
Non-Pharmacological Therapies for Post-exertional Malaise (PEM) and Fatigue
Pacing of physical and cognitive activity to conserve energy and minimize post-exertional malaise (1). Once the patient has achieved a stable baseline using pacing, then very carefully selected and individualized increases in activity can be undertaken. The type of activity must be tailored for the patient’s level of severity and to ensure the activity does not trigger post-exertional malaise.
Assistive devices, such as a motorized scooter, wheelchair, walker with seat/basket, shower chair, handicap parking sticker, audio recorders and recording pens, etc. when needed to conserve energy. Home health aides for those who are more severely ill.
Ear plugs, eye masks, and sunglasses, blue light filters, perfume free environments, etc to decrease sensory stimulation. May need to maintain low sensory environment for most severely ill.
School or work accommodations such as flexible hours, shortened days, periodic breaks and place to lay down during breaks, lighting and other environmental modifications to avoid sensory overload and conserve energy.
Non-Pharmacological Therapies for Orthostatic Intolerance
- Salt, fluid loading, electrolytes, IV saline. Sodium intake should be complemented with modest potassium, magnesium supplements. Camelbacks for hydration
- Compression stockings or abdominal binder.
- Positional changes: Avoid prolonged sitting or standing. Knees higher than hips. Sit on legs so legs are not hanging down.
- Consistent, carefully tailored exercise, as long as the patient can do so without triggering PEM. May need to do exercise lying down, seated, or in water.
- Treat comorbidities that may contribute to orthostatic intolerance.
Non-Pharmacological Therapies for Sleep Issues
- Sleep hygiene practices are a part of treatment but may be marginally effective in most patients. Recommendations may need to be tailored for bedbound patients and those who need to be recumbent to minimize symptoms such as orthostatic intolerance.
- Meditation and relaxation exercises.
- Ear plugs and eye mask.
- Light therapy. Retimer Light therapy glasses. Sunlight for 15 minutes upon waking.
- Blue light filters to filter out blue light from phones and computers
Non-Pharmacological Therapies for Gastrointestinal Issues
Healthy, varied diet low in processed food. Dietary changes and elimination of certain foods that provoke symptoms. Many patients do better avoiding foods such as caffeine, alcohol, spicy foods, aspartame, sugar, possibly dairy and gluten.
Non-Pharmacological Therapies for Cognitive dysfunction
- Cognitive pacing (e.g. only focus on one task at a time, limit reading time)
- Simple memory aids (e.g. calendar reminder systems, notes, etc.)
- Positional changes: Perform cognitive functions lying down and stay hydrated if orthostatic intolerance is a problem
- Caffeine or short acting stimulants if well tolerated
Non-Pharmacological Therapies for Pain
- Pacing to avoid flare up of pain
- Hot or cold packs as needed to relieve the specific source of pain
- Physical therapy, Massage, Myofascial release, Acupuncture, Dry needling of trigger points
- Chiropractic treatments
- Meditation and relaxation
- Neurofeedback techniques may be helpful
Currently, there are no treatments approved specifically for ME/CFS and Long Covid. But there are a number of pharmacological and non-pharmacological treatments that a clinician can use to help reduce the severity of specific symptoms and improve the patient’s quality of life. Depending on a patient’s presentation and testing, the treatment recommendations above are those used by ME/CFS clinical experts to treat various aspects of ME/CFS, such as orthostatic intolerance, sleep issues, pain, and immune function. Recommendations for supplements are not provided in this article.
Some disease experts are evaluating the selective use of antivirals and immune modulators in ME/CFS and have seen evidence of efficacy in some patients. Double blind randomized controlled treatment trials are needed to evaluate these therapies. A specialty consultation may be helpful in identifying and treating these or other aspects of the disease.
Some ME/CFS patients have increased intolerance to a variety of medications. In these patients, drugs should be started at low doses and increased slowly to avoid triggering drug sensitivities common in ME/CFS. Clinicians should also be aware of any potential impact of ingredients considered to be inactive in medications (e.g. fillers, vehicles, preservatives). For patients sensitive to drug fillers, the physician might speak with a compounding pharmacy to determine if a liquid preparation is an alternative.
Comorbidities should also be diagnosed and treated using the published standard of care. Doing so can also help decrease the symptom burden and improve the patient’s quality of life. Recommendations for treatment of comorbidities are not covered here.
The treatment recommendations provided here are general ones. In deciding on the specific treatment approach, the treating physician should consider the presentation and needs of the individual patient along with up-to-date drug product information for approved uses, dosages, and risks of specific treatments for specific indications.
References
- mecfscliniciancoalition.org
- Crosby, L.D., Kalanidhi, S., Bonilla, A. et al. Off label use of Aripiprazole shows promise as a treatment for Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS): a retrospective study of 101 patients treated with a low dose of Aripiprazole. J Transl Med 19, 50 (2021). https://doi.org/10.1186/s12967-021-02721-9
- Leitzke M. Is the post-COVID-19 syndrome a severe impairment of acetylcholine-orchestrated neuromodulation that responds to nicotine administration? Bioelectron Med. 2023 Jan 18;9(1):2. doi: 10.1186/s42234-023-00104-7. PMID: 36650574; PMCID: PMC9845100. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9845100/