An 81-year-old woman with cerebrovascular disease presented to the emergency department with a 1-week history of vomiting.
Findings on abdominal examination were notable for normal bowel sounds and the absence of tenderness, rebound, or guarding.
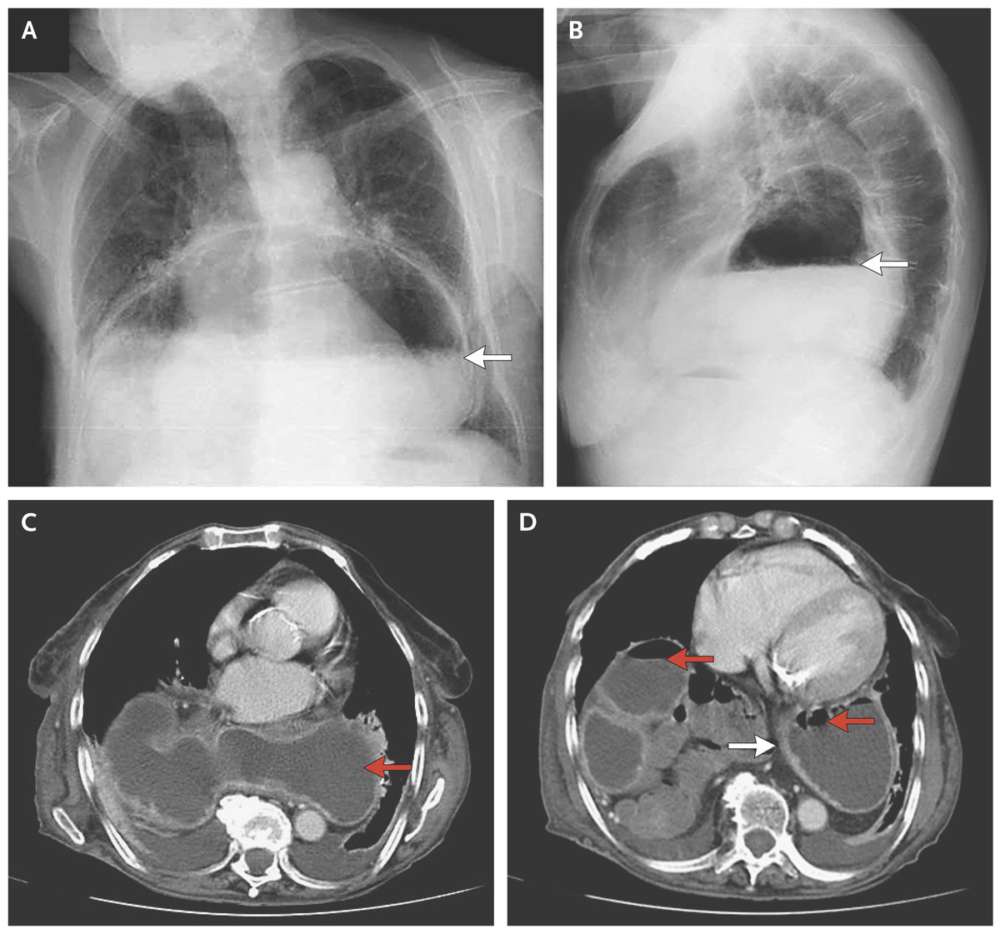
A chest radiograph showed a large air–liquid shadow in the inferior retrocardiac position (Panels A and B, arrows), which suggested a large paraesophageal hernia.
A computed tomographic scan showed a large retrocardiac mass containing air and liquid (Panels C and D, red arrows) that was consistent with herniation of the stomach into the chest.
Thickening of the gastric wall suggested edema (Panel D, white arrow) and compression of the first portion of the duodenum, which caused gastric distention.
Hiatal hernias are defined as protrusion of the stomach through the diaphragm into the chest. The degree of displacement can produce obstructive symptoms, as occurred in this patient, and may increase the risk of volvulus.
Owing to her generally poor health status, the patient was treated conservatively, with gastric suction performed through a nasogastric tube followed by initiation and advancement of her oral diet, first with clear liquids, then soft foods, and finally solid foods. The vomiting resolved, and the patient was asymptomatic at the time of discharge.