Table of Contents
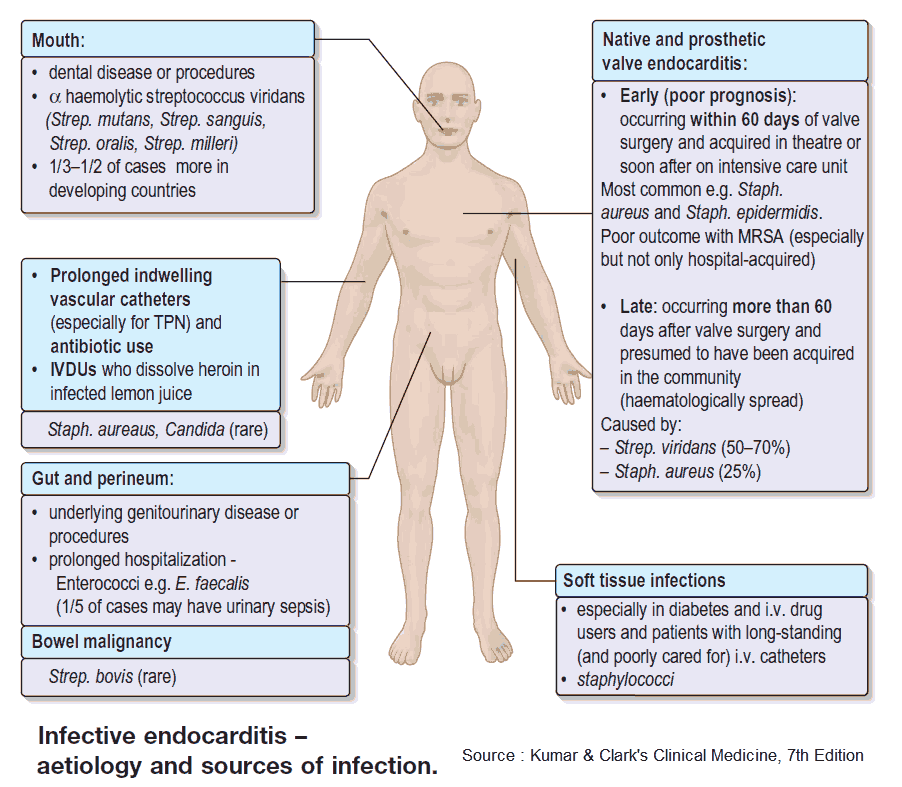
Infective endocarditis (IE) is a bacterial or fungal infection of the heart valves or perivalvular structures and is a highly morbid condition associated with significant in-hospital mortality. The morbidity of IE is mediated through direct effects on the heart and embolic complications.
- Direct cardiac effects of Infective Endocarditis include:
- Valve incompetence
- Perivalvular abscesses
- Conduction abnormalities
- Heart failure.
- Noncardiac sequelae of Infective Endocarditis result from embolization of vegetation fragments to select organs.
- Timely diagnosis of Infective Endocarditis and IE-related cardiac dysfunction is imperative to prevent increased morbidity and mortality.
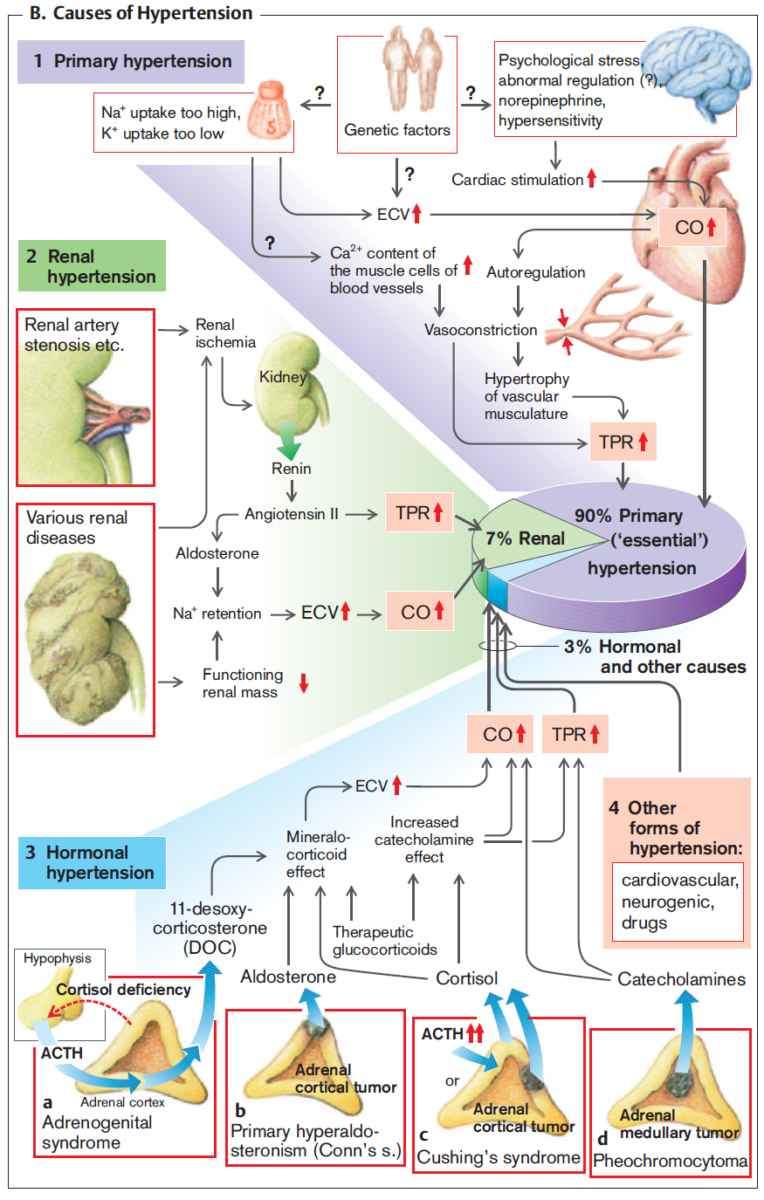
Presentation of Infective Endocarditis
The presentation of Infective Endocarditis can be subtle. Often, patients will present with symptoms attributable to multiple organ systems. The majority of patients will have a fever upon presentation.
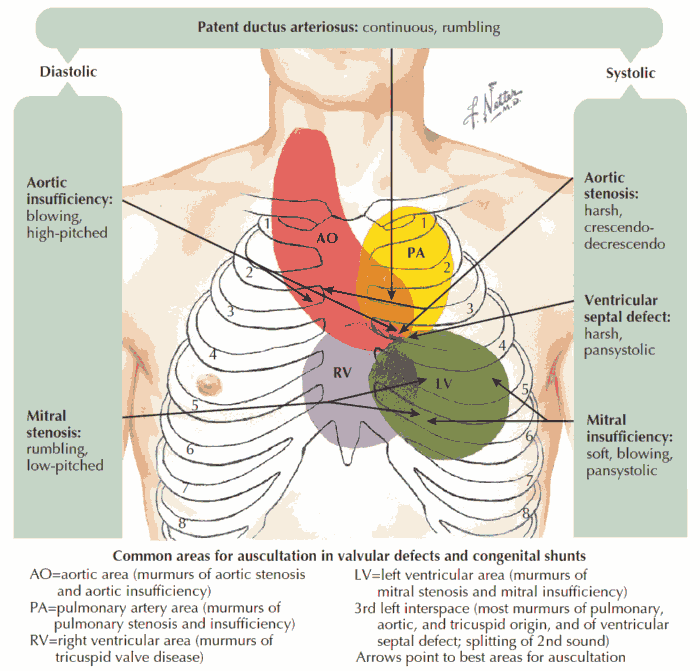
The presence of a new heart murmur has been shown to be a sensitive finding in patients with Infective Endocarditis.
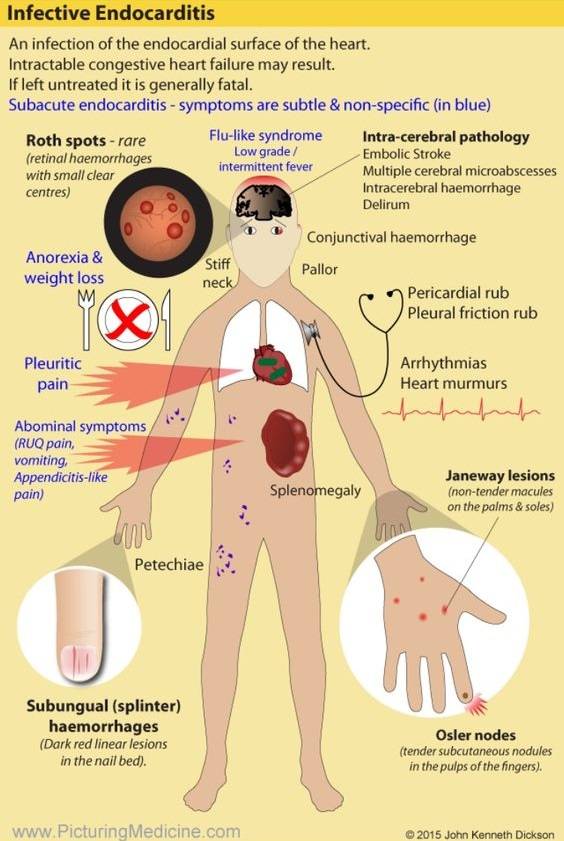
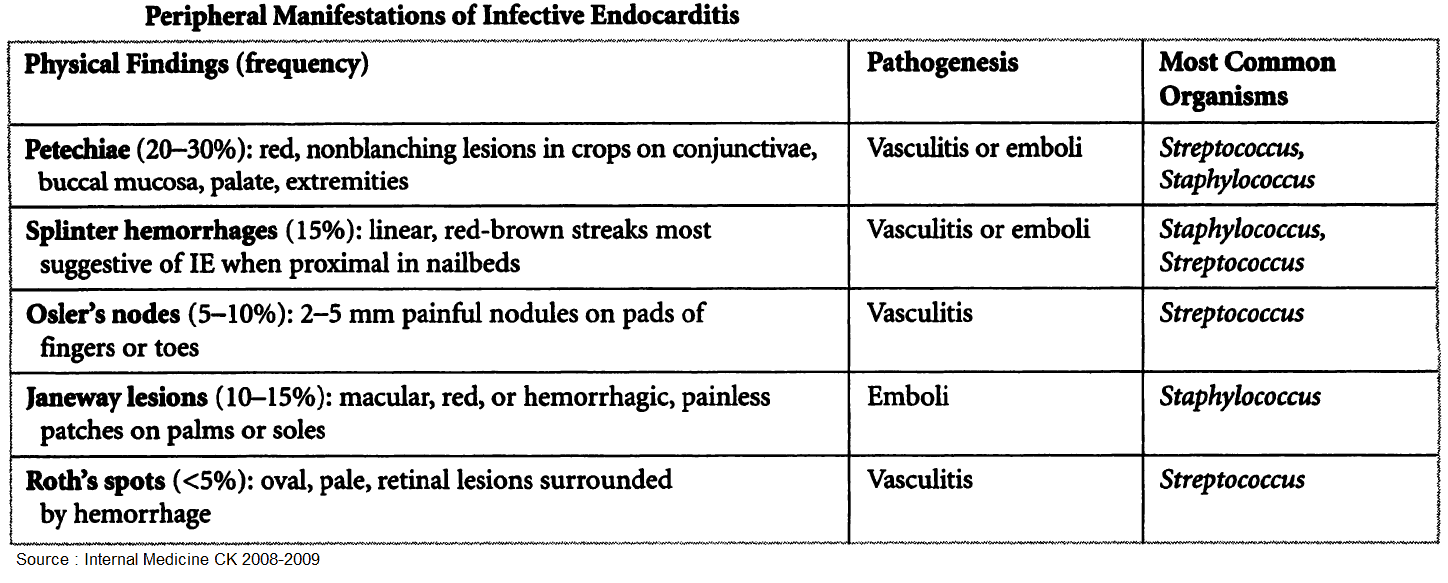
Classic signs of Infective Endocarditis such as Osler nodes, Janeway lesions, and Roth spots are infrequently seen. The Duke Criteria can be used for timely diagnosis and risk stratification of patients with Infective Endocarditis.
Septic Embolization in Patients with Infective Endocarditis
- Septic embolization occurs in many patients with Infective Endocarditis and is due to fragmentation of a valvular vegetation.
- Risk factors for embolization include:
- Diabetes
- Age
- Vegetation length
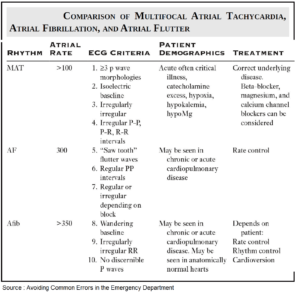
- Atrial fibrillation
- IE due to Staphylococcus aureus.
- The predominant organs affected by septic embolization depend on the affected heart valve.
- Infective Endocarditis that involves the mitral or aortic valve more frequently embolizes to the brain, spleen, liver, kidneys, and musculoskeletal system.
- Infective Endocarditis that affects the tricuspid valve usually embolizes to the lungs.
- Right to left shunts, such as those found with a patent foramen ovale, can result in paradoxical septic embolization.
Tricuspid Valve Infective Endocarditis
- Tricuspid valve Infective Endocarditis is typically found in:
- Intravenous drug abusers (IVDA)
- Patients with indwelling venous catheters
- Patients with automated implantable cardiac defibrillators or pacers.
- Characteristically, patients with tricuspid valve Infective Endocarditis have a fever and respiratory symptoms.
- A chest x-ray (CXR) typically demonstrates multiple areas of opacities. Computed tomography (CT) is more sensitive than CXR in diagnosing pulmonary septic emboli. These are often seen as numerous peripheral nodules on CT.
Mitral or Aortic Valve Infective Endocarditis
- Mitral or aortic valve Infective Endocarditis is more predominant in the general population than is tricuspid valve Infective Endocarditis.
- Central nervous system (CNS) embolization can occur in up to 20% and often precedes the diagnosis of Infective Endocarditis. Risk of cerebral embolism is higher with mitral valve involvement and S. aureus IE.
- The clinical manifestations depend on the extent and location of the embolic lesions. The territory supplied by the middle cerebral artery is the most common location for embolic lesions. CNS embolization can manifest as an ischemic stroke, hemorrhagic stroke, transient ischemic attack, or simply asymptomatic lesions found on imaging.
- Less common clinical manifestations include embolic meningitis and mycotic aneurysms. Diagnosis of acute neurologic changes must occur within the context of the presentation.
- Acute neurologic symptoms in the setting of a fever and heart murmur should raise suspicion for cerebrovascular embolization.
- The risk of CNS embolization decreases once antibiotics are administered.
Involvement of the Cronary Arteries in Infective Endocarditis
Involvement of the coronary arteries is a potentially deadly sequela of Infective Endocarditis. Perivalvular abscess formation can develop and lead to extrinsic compression of the coronary arteries.
Mitral valve vegetations can embolize to the coronary arteries and lead to an acute coronary syndrome. This, too, generally occurs in a clinical scenario that suggests Infective Endocarditis.
In the setting of ECG changes consistent with a STEMI, urgent revascularization is still required.
Organ Abscesses
The presence of hepatic or splenic abscesses found on imaging should raise suspicion for Infective Endocarditis. Embolization to the kidneys can also lead to abscess formation and bacteriuria. The presence of S. aureus in a patient without indwelling catheters and without recent instrumentation should raise suspicion for Infective Endocarditis.
It is important for providers to be familiar with the prevalence of Infective Endocarditis in their population. Lesions suspicious for embolic phenomenon can be an important clue in making an early diagnosis of IE and avoidance of further complications.
Key Points
- Timely diagnosis of Infective Endocarditis can reduce morbidity and mortality.
- IE can cause significant organ dysfunction through embolization of vegetation fragments.
- Tricuspid valve IE often causes septic pulmonary emboli.
- Mitral or aortic valve IE can embolize to the CNS, liver, spleen, or kidneys.
- Consider IE in the patient with acute CNS symptoms, fever, and a new heart murmur.