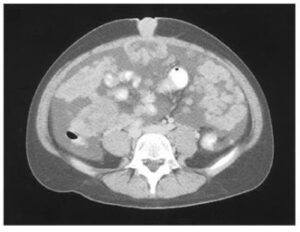
On physical examination, she had a generalized, macular, nonblanching rash in a reticular pattern with purplish discoloration consistent with livedo reticularis.
Because of the spontaneous agglutination of the blood, the blood samples were warmed in a saline bath at 37°C.
Laboratory evaluation revealed a hematocrit of 14% (reference range, 34 to 46), an indirect bilirubin level of 7.6 mg per deciliter (reference value, <1.0), and a lactate dehydrogenase level of 1298 U per liter (reference range, 100 to 190).
The direct antiglobulin test was positive for the complement component C3, and the test for cold agglutinins was positive at a 1:2048 dilution at 4°C.
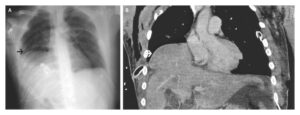
A diagnosis of cold agglutinin disease, a form of acquired autoimmune hemolytic anemia, was made, a condition that may have been exacerbated by the patient’s recent viral infection along with the cold weather in upstate New York, where the temperature was 15°F (−9°C) at the time of her presentation.
The patient was warmed and treated with blood transfusions and rituximab for 1 week. At the time of hospital discharge, she had a hematocrit of 30% and a reduction in dizziness, but the rash persisted.