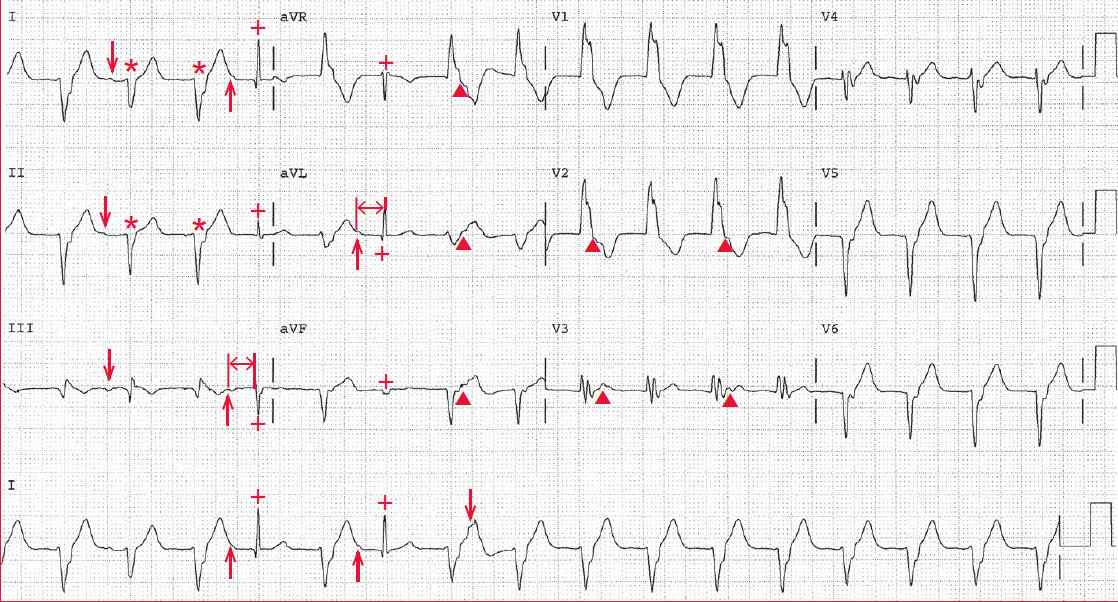
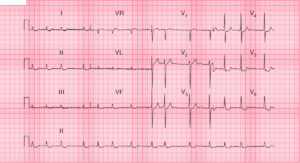
The ECG shows a regular rhythm at a rate of 100 bpm. The QRS complex duration is prolonged (0.16 sec) and the axis is indeterminate, between –90° and +/ -180° (negative QRS complex in leads I and aVF).
Two narrow QRS complexes (+) (duration 0.08 sec) are preceded by P waves (↑) with the same PR interval (↔) of 0.24 second. These are, therefore, sinus complexes.
Although no other P waves are clearly obvious, there appears to be a P wave (↓) in leads I and III between the first and second QRS complexes. Also noted are ST-T wave irregularities, especially obvious in leads V2-V3 (▲), that are suggestive of P waves.
In addition, there are subtle differences in QRS complex morphology (*), especially obvious in leads I and II. These findings indicate AV dissociation, and the narrow sinus complexes (+) represent intermittent capture or Dressler complexes.
Hence this rhythm has a number of features consistent with a diagnosis of sustained ventricular tachycardia; that is, the presence of AV dissociation is confirmed by the occurrence of occasional captured sinus beats (Dressler complexes) and probably a fusion beat (second QRS complex, which is preceded by a P wave [↓] with a short PR interval and a slight change in QRS complex morphology).
Captured and fusion complexes result from an impulse conducting through the AV node that fuses with an impulse generated in the ventricular myocardium.
Two other features confirm ventricular tachycardia. First is the presence of an indeterminate axis, which indicates that impulse conduction is not via the normal His-Purkinje system but results from direct myocardial activation. This is seen with a ventricular complex, paced complex, or preexcited complex (ie, Wolff- Parkinson-White).
Second, non–rate-related changes in ST-T waves and slight changes in QRS complex morphology can confirm ventricular tachycardia. The subtle changes in QRS complex morphology and ST-T waves are due to the fact that with ventricular tachycardia ventricular activation is not via the normal His-Purkinje system (in which case the fixed pathway for activation would result in uniform QRS complexes) but is by direct myocardial activation (in which the pattern of conduction may change). The changes in the ST-T waves reflect changes in ventricular repolarization or superimposed P waves.
Importantly, any superventricular rhythm (sinus, atrial, or AV nodal) always conducts to the ventricle through the same pathway; hence the QRS complexes and ST-T waves are identical.
As all of the QRS complexes are similar in morphology (although with slight changes in appearance), this is monomorphic ventricular tachycardia.
This wide complex tachycardia has a QRS complex morphology that resembles a right bundle branch block (R-wave amplitude taller than S-wave depth in lead V1). The lack of an RSR′ pattern in lead V1 and the presence of S > R in lead V6 are both consistent with the diagnosis of ventricular tachycardia.