Ventricular tachycardia is a wide complex tachycardia (WCT) that is typically associated with coronary artery disease or other significant heart disease.
The rapid rate, often in conjunction with poor baseline cardiac function, can produce cardiovascular instability. If this instability is not promptly treated, cardiovascular collapse will almost certainly ensue.
This has led to the position of treating all WCTs as ventricular tachycardia (VT) until proven otherwise.
For management purposes, it is important to attempt to differentiate between VT and supraventricular tachycardia (SVT) with aberrant conduction.
READ ALSO : Never Mistake Ventricular Tachycardia for Supraventricular Tachycardia with Aberrant Conduction
In some cases, the distinction between these two rhythms is not possible. As a result, management decisions must be made based upon the patient’s clinical situation and the electrocardiography (ECG) rhythm.
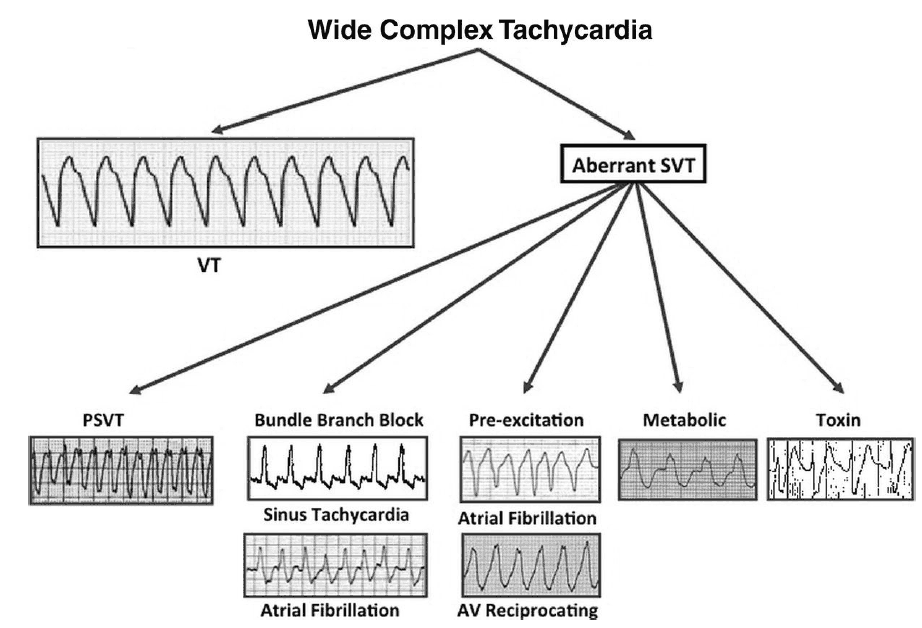
Mimics of Ventricular Tachycardia
There are numerous conditions that can mimic the appearance of VT on the ECG. These include, but are not limited to:
- SVT with aberrant conduction
- sinus tachycardia
- atrial fibrillation
- atrial flutter
- paroxysmal SVT
- multifocal atrial tachycardia
- Wolff-Parkinson-White syndrome
- Artifact
- Metabolic disorders (i.e., hyperkalemia)
- Toxic ingestions (i.e., medications that block the sodium channel).
In some of these conditions, the electrical impulse is delayed, or slowed, as it passes through the conduction system and ventricular myocardium. This results in a wide QRS complex.
The dysfunction in the intraventricular conduction system can be permanent or temporary. In some cases, abnormal conduction may only be seen at higher heart rates.
SVT with aberrant conduction
Due to the presence of a bundle branch block (BBB), SVTs due to these rhythms will demonstrate a wide QRS complex.
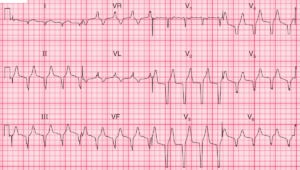
Wolff-Parkinson-White syndrome (WPW)
Wolff-Parkinson-White syndrome (WPW) is a form of ventricular preexcitation that involves an accessory conduction pathway between the atria and ventricles.
WPW patients are prone to develop a variety of supraventricular tachyarrhythmias, especially WPW-related atrial fibrillation and WCT.
Hyperkalemia
Severe hyperkalemia can also cause a rapid, wide complex rhythm that can easily be mistaken for VT. Hyperkalemia should be considered in any WCT where the heart rate is <120 beats per minute (bpm).
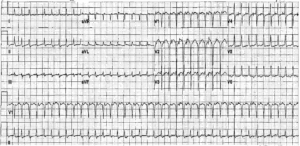
Sodium Channel Blockers
Medications that block the sodium channel (i.e., tricyclic antidepressants) produce a WCT that is often mistaken for VT.
In the case of hyperkalemia or sodium channel blocker toxicity, the administration of sodium bicarbonate can be both diagnostic and therapeutic.
READ ALSO : Know When to Administer Sodium Bicarbonate in the Critically ill Poisoned Patient
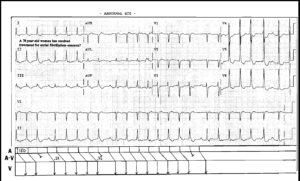
Sinus tachycardia
Sinus tachycardia with an anterior ST-segment elevation myocardial infarction can mimic VT.
ECG artifact
Lastly, ECG artifact can be mistaken for VT. Patient movement, poor electrode application, equipment malfunction, or electromagnetic interference can all cause ECG artifact and mimic the appearance of VT.
Key Points
- SVT with aberrant conduction is a common mimic of VT.
- Consider hyperkalemia in any WCT where the heart rate is <120 bpm.
- Tricyclic antidepressant toxicity is well known to cause a WCT and should be considered in the differential diagnosis of VT.
- Patient movement, equipment malfunction, and poor electrode placement or contact cause result in artifact and mimic the appearance of VT.
- Consider WPW in the differential diagnosis of a WCT.
Suggested Readings
- deSouza IS, Peterson AC, Marill KA, et al. Differentiating types of wide-complex tachycardia to determine appropriate treatment in the emergency department. Emerg Med Pract. 2015;17:1–22.
- Jastrzebski M, Kukla P, Czarnecka D, et al. Comparison of five ectrocardiographic methods for differentiation of wide-QRS tachycardias. Europace. 2012;14:1165–71. https://academic.oup.com/europace/article/14/8/1165/464643
- Mattu A. ECG Pearls: beware the slow mimics of ventricular tachycardia. Emergency Physicians Monthly August 24, 2010. Available at: http://epmonthly.com/article/ecg-pearls-beware-the-slow-mimics-ofventricular-tachycardia . Accessed July 1, 2016.