This article is an answer to the ECG Case 171
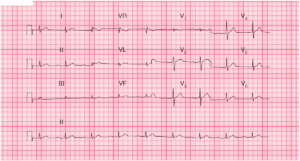
There is a regular rhythm at a rate of 124 bpm. There is a P wave (+,++) before each QRS complex with a stable PR interval (0.20 sec). The P waves are positive in leads I, II, aVF, and V4–V6. Hence this is a sinus tachycardia.
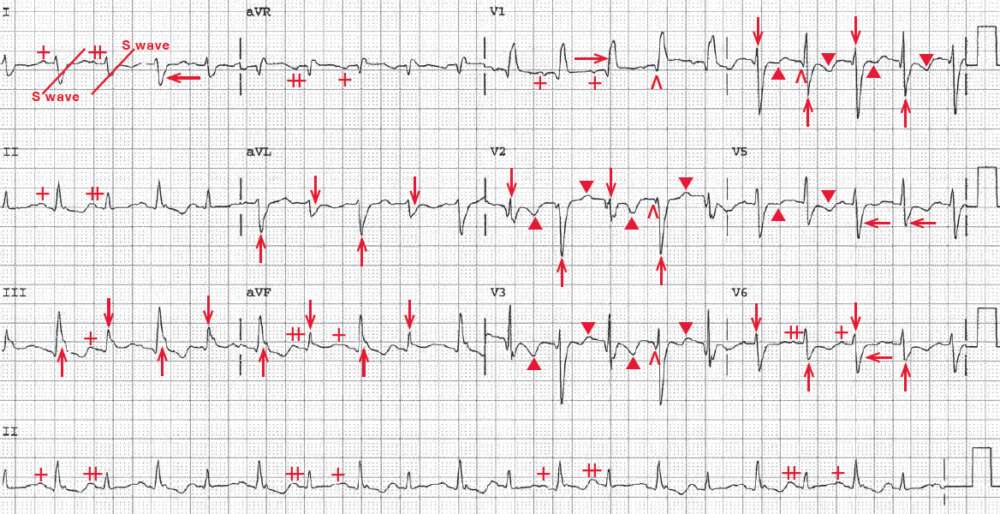
The QRS complex duration is prolonged (0.16 sec) and there is a RBBB morphology with a broad terminal R wave in lead V1 (→) and broad S wave in leads I and V4–V6) (←). The axis is rightward between +90° and +180° (negative QRS complex in lead I and positive in lead aVF), even when the terminal S wave due to the RBBB is considered.
There is no evidence for a lateral wall myocardial infarction (there is an rS morphology in leads I and aVL), right ventricular hypertrophy (which cannot be diagnosed in the presence of a RBBB), Wolff-Parkinson-White pattern (short PR and delta wave), right-left arm lead switch (negative P wave and T wave in leads I and aVL and positive P, QRS and T wave in lead aVR), or dextrocardia (resembling right-left arm lead switch and also with reverse R-wave progression). Hence this is a left posterior fascicular block.
There are initial Q waves (^) in leads V1–V4, diagnostic of an old anterior wall myocardial infarction. The QT/QTc intervals are prolonged (360/520 msec) but are normal when the prolonged QRS complex duration is considered (300/430 msec).
Noted are beat-to-beat changes in QRS amplitude (↓, ↑); this is electrical or QRS alternans. Also noted are beat-to-beat changes in T wave (▲, ▼) as well as P-wave amplitude (+, ++); hence there is T and P-wave alternans.
Based on the presenting symptoms and the physical examination, the occurrence of electrical alternans in this case is due to a large pericardial effusion and cardiac tamponade, which causes a swinging of the heart with each beat in a fluid-filled pericardial sac (pendulum effect). Hence there are anatomic changes in the location of the heart.
In this situation, there is QRS and T-wave alternans present as well as P-wave alternans. Electrical alternans, which can only be diagnosed when the rhythm is regular, may also be seen with other conditions, including any rapid, regular supraventricular tachycardia (atrial tachycardia, atrial flutter, atrioventricular nodal reentrant tachycardia [AVNRT], or atrioventricular reentrant tachycardia [AVRT]), associated with a preexcitation syndrome, an acute myocardial infarction, a dilated cardiomyopathy, or decompensated heart failure.
In these situations, QRS and T-wave alternans are a result of beat-to-beat changes in calcium influxes into the ventricular myocardium. The atrial myocardium is not affected. As there is no change in the anatomic position of the heart, P-wave alternans is not seen in these situations. It has been reported that it may also be seen with ventricular tachycardia, but this is probably very uncommon. The forms of ventricular tachycardia in which it may be seen are a fascicular tachycardia or a right ventricular outflow tachycardia.
READ MORE: ECG Interpretation – All you need to know
SIMILAR CASE: Pericardial Effusion / Tamponade