ECG Interpretation
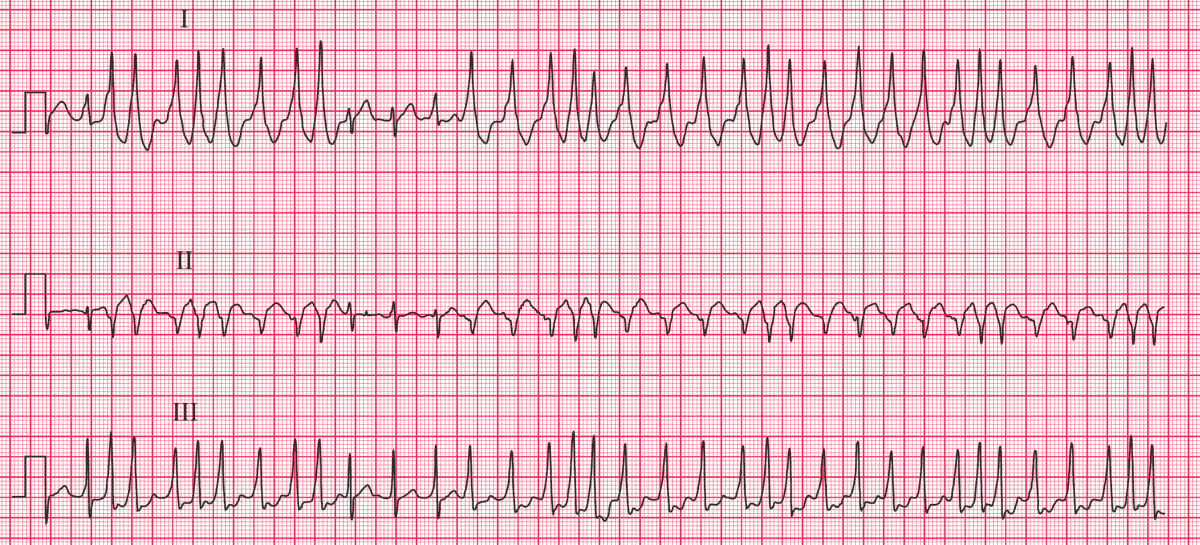
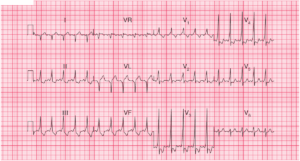
The ECG 1 shows:
- A very irregular tachycardia with a ventricular rate of up to 200/min
- No visible P waves
- A few normal complexes, but the majority are wide and have a slurred upstroke
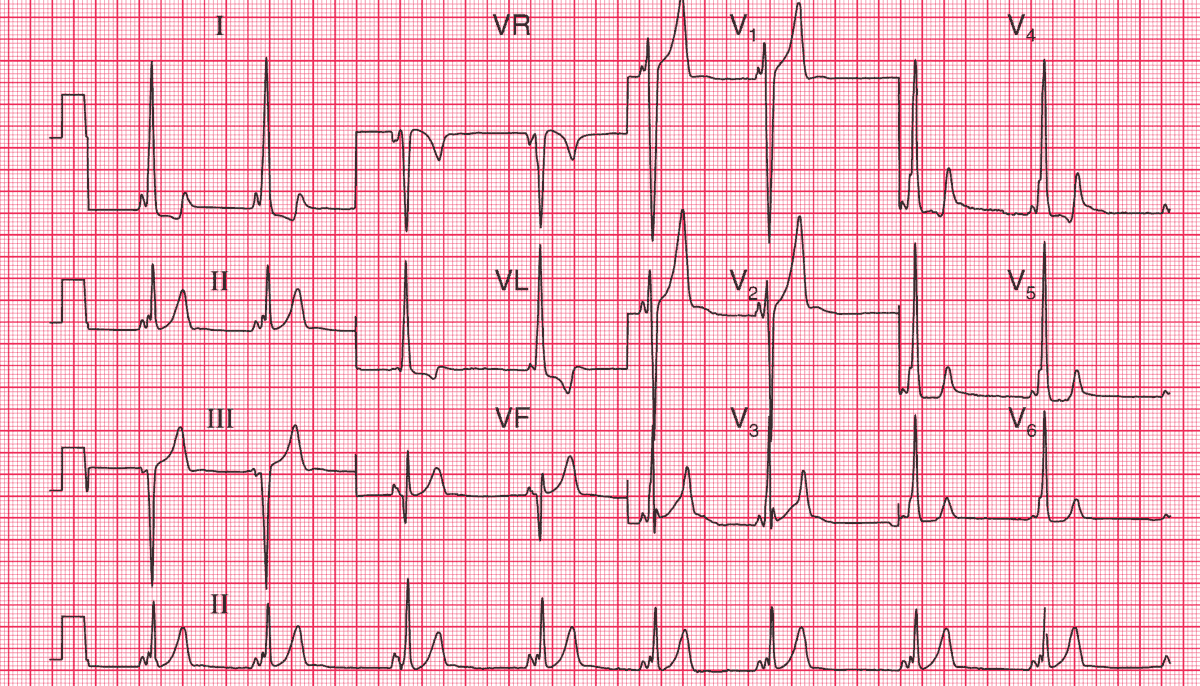
The ECG 2 (recorded when he was asymptomatic) shows:
- Sinus rhythm, rate 51/min
- Very short PR interval
- Normal axis
- Bizarre and widened QRS complexes with a slurred upstroke (delta wave), best seen in leads I and V4–V6
Clinical Interpretation
This is the Wolff–Parkinson–White (WPW) syndrome: the accessory pathway is on the right side, and this is sometimes called ‘type B’. The irregular tachycardia is due to atrial fibrillation.
What to do ?
Atrial fibrillation in the WPW syndrome can lead to sudden death due to ventricular fibrillation, so ablation of the abnormal pathway is needed urgently.
Immediate treatment of the atrial fibrillation should be by cardioversion if there is haemodynamic compromise.
Digoxin, verapamil and diltiazem should be avoided because these block the atrioventricular node and encourage conduction through the accessory pathway.