Table of Contents
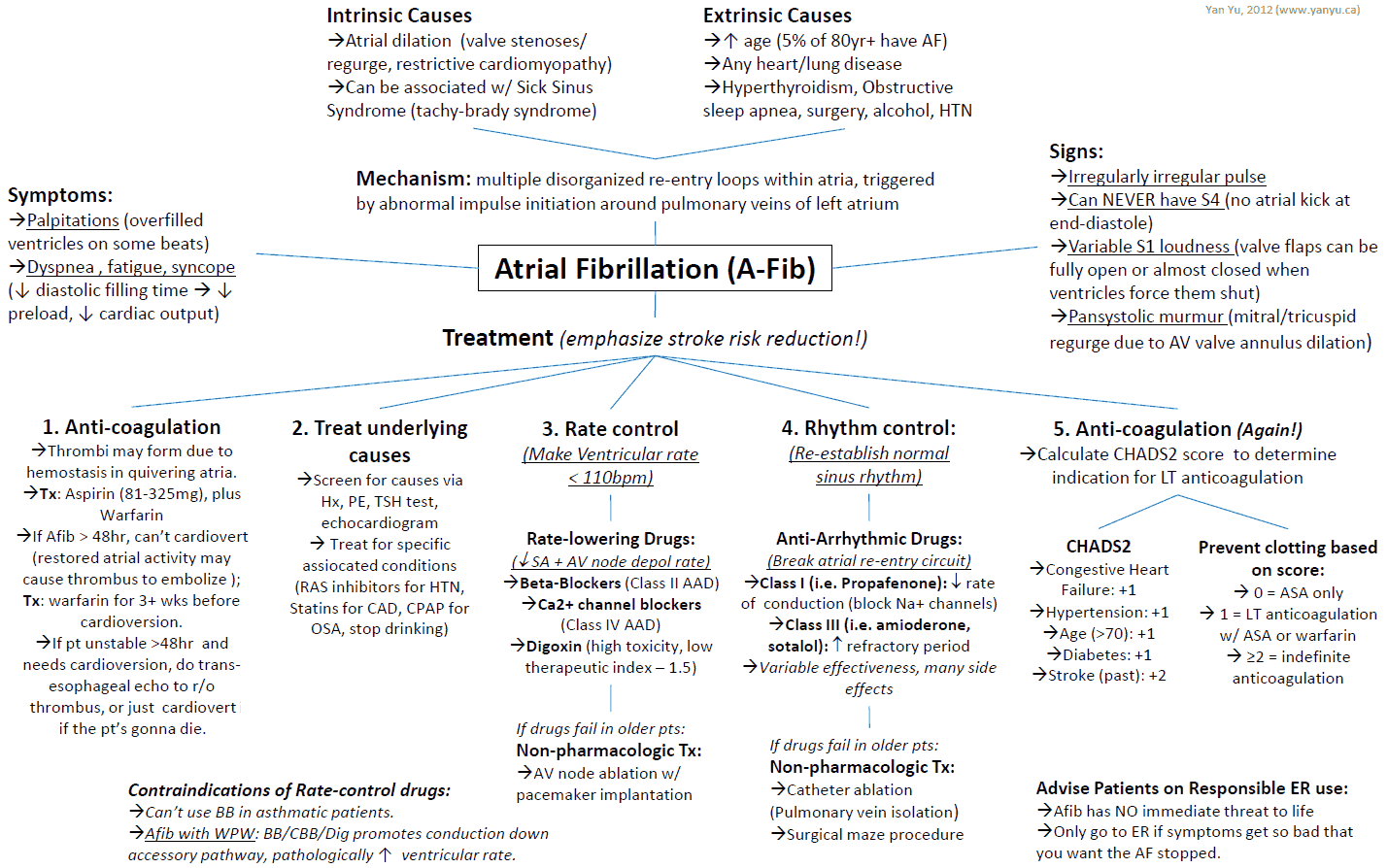
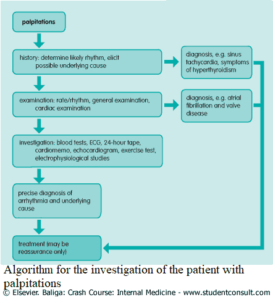
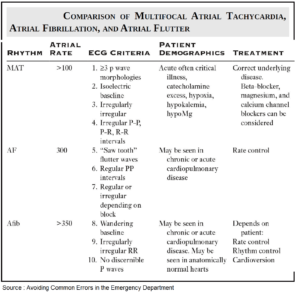
Atrial fibrillation with a rapid ventricular response (RVR) is a common condition in emergency department (ED) patients. In the initial assessment of patients with atrial fibrillation and an RVR, it is critical for the emergency provider (EP) to determine if the patient is stable or unstable. In addition, it is also important for the EP to determine if the instability is due to the RVR or is secondary to a nonarrhythmic event.
Management of Hemodynamic instability due to Rapid Ventricular Response (RVR)
Patients with atrial fibrillation who are unstable due to an RVR should be treated with synchronized cardioversion.
Management of Hemodynamic instability due to nonarrhythmic process
Patients with atrial fibrillation who are unstable due to a nonarrhythmic process (i.e., sepsis, hypovolemia, alcohol withdrawal, pulmonary embolism) should receive treatment targeted to the primary event. In some of these patients, cardioversion may still be necessary while treating the primary disorder.
Management of Hemodynamic stable patients with atrial fibrillation and RVR
For stable patients with atrial fibrillation and an RVR, the EP must decide upon appropriate pharmacologic therapy to control the heart rate.Selection of the appropriate medication to control heart rate requires careful consideration of the clinical presentation, patient comorbid conditions, and current medications. Comorbid conditions such as congestive heart failure (CHF) impact the selection of medications used for rate control.
Medications commonly used to control heart rate in atrial fibrillation include :
1. Calcium Channel Blockers
A nondihydropyridine CCBs, such as diltiazem or verapamil, is considered first-line therapy for rate control of atrial fibrillation. CCBs target the atrioventricular (AV) node and suppress cardiac conduction.
Importantly, CCBs are contraindicated for the treatment of atrial fibrillation in the setting of severe left ventricular dysfunction and in patients with Wolff-Parkinson-White (WPW) syndrome, where conduction is through the accessory pathway.
Diltiazem
Diltiazem is the recommended CCB for atrial fibrillation with an RVR. The initial dose of diltiazem is 0.25 mg/kg administered intravenously over 2 to 5 minutes. A decrease in heart rate should be seen in ~5 to 10 minutes. If there is no response, a second dose of diltiazem at 0.35 mg/kg may be given 15 to 30 minutes after the initial dose. Diltiazem can be given as a continuous infusion. The infusion is started at 5 mg/hour and can be gradually increased to 15 mg/hour based on the clinical response.
Verapamil
Verapamil can also be used to control heart rate in atrial fibrillation. The dose of verapamil is 0.075 to 0.15 mg/kg administered intravenously over 2 to 5 minutes. The onset of action of verapamil is generally within 2 minutes of intravenous administration. Additional doses can be given every 15 to 30 minutes, as needed. A continuous infusion of verapamil can be initiated at 0.005 mg/kg/minute.
2. Beta-Adrenergic Blockers
Beta-adrenergic blockers can also be used to control heart rate in patients with atrial fibrillation and an Rapid Ventricular Response (RVR). Beta-adrenergic blockers control heart rate through a decrease in sympathetic tone. The most common beta-blockers used in the ED are metoprolol, propranolol, and esmolol.
There is no significant literature that demonstrates superiority of any one beta-adrenergic blocker. Contraindications to beta-adrenergic blocker use include hypotension, severe CHF, pulmonary edema, and severe obstructive lung disease.
Metoprolol
Metoprolol is often the initial beta-blocker used in the management of the atrial fibrillation patient with RVR. The initial dose of metoprolol is 2.5 to 5 mg administered intravenously over ~2 minutes. Additional doses can be given every 5 minutes until a cumulative dose of 15 mg is reached. A dose of 25 mg of immediate release, or 50 mg of extended release, metoprolol can be administered as a transition to oral therapy once heart rate control is achieved.
Propranolol
If propranolol is chosen, it can be given as an initial dose of 1 mg intravenously over 1 minute, with repeated doses of 1 mg every 2 minutes until a total of 3 mg has been given. Additional doses of propranolol can be given but should not be administered for ~4 hours from the last dose.
Esmolol
Esmolol has the shorted duration of effect and, therefore, is of significant value when beta-blocker-related hemodynamic tolerance is a concern. Esmolol can be administered as an initial bolus of 0.5 mg/kg infused over 1 minute, followed by a continuous infusion of 50 mcg/kg/minute. The maintenance infusion of esmolol typically ranges between 50 mcg/kg/minute and 300 mcg/kg/minute.
3. Digoxin
Digoxin is considered a second-line agent for rate control in the patient with atrial fibrillation and RVR. Digoxin should be considered in patients unable to tolerate beta-adrenergic blockers or CCBs, such as those with acute CHF exacerbations or hypotension. Digoxin lacks the efficacy of first-line agents due to a slower onset of action and a weaker potency to block the AV node.
The initial dose of digoxin is 0.25 mg administered intravenously every 2 hours to a maximum of 1.5 mg in 24 hours. The time of onset of digoxin ranges between 15 and 30 minutes, though significant rate control may not be seen for 6 to 12 hours.
4. Amiodarone
Amiodarone has been used to maintain sinus rhythm in patients with atrial fibrillation. It can also be used to control heart rate in atrial fibrillation patients with an RVR. Similar to digoxin, amiodarone can be considered in hypotensive patients and those with acute decompensation of CHF.
The initial dose of amiodarone for this indication is 150 mg administered intravenously over 10 to 20 minutes. This dose can then be followed by an additional intravenous dose of 150 mg if adequate rate control has not been achieved within 60 minutes. A maintenance infusion of amiodarone can be started at 1 mg/minute for 6 hours, followed by 0.5 mg/minute for an additional 18 hours.
Atrial fibrillation with RVR in Wolff Parkinson White (WPW)
WPW with accessory pathway conduction must be considered in atrial fibrillation patients with an RVR where the QRS is wide with varied morphologies. In this special situation, the use of all AV node–blocking agents should be avoided and the patient treated with synchronized cardioversion or intravenous procainamide.
READ MORE about: Atrial Fibrillation in the Wolff-Parkinson-White (WPW) Syndrome
Key Points
- Patients with atrial fibrillation who are unstable due to an RVR should be treated with synchronized cardioversion.
- Diltiazem, at a dose of 0.25 mg/kg, is the first-line medication for most patients with atrial fibrillation with an RVR.
- All AV node–blocking medications are contraindicated for rate control of atrial fibrillation in the setting of WPW, where conduction occurs through the accessory pathway.
- Contraindications to the use of beta-blockers in the treatment of atrial fibrillation include hypotension, severe CHF, severe COPD, and acute asthma exacerbation.
- Consider digoxin for rate control in the patient with hypotension or an acute exacerbation of CHF.