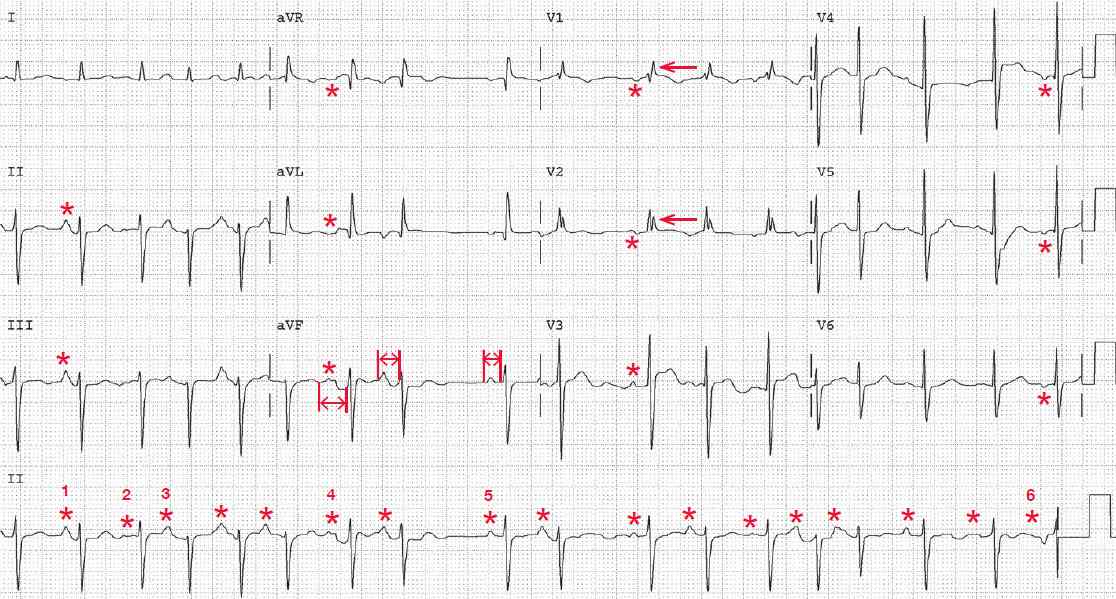
The rhythm is irregularly irregular at an average rate of 108 bpm. There are only three supraventricular arrhythmias that are irregularly irregular:
- sinus arrhythmia in which there is one P-wave morphology and PR interval
- multifocal atrial rhythm (wandering atrial pacemaker) with a rate less than 100 bpm or multifocal atrial tachycardia with a rate greater than 100 bpm in which there are three or more different P-wave morphologies and no P-wave morphology is dominant
- atrial fibrillation, in which there is no organized atrial activity but there are fibrillatory waves.
There is atrial activity, and a P wave (*) is seen before each QRS complex. However, at least three different P-wave morphologies (and no one dominant morphology) can be seen as well as variability in the PR interval (↔). Hence this is multifocal atrial tachycardia.
The QRS complexes are of normal duration (0.08 sec). The axis is extremely leftward, between –30° and –90° (positive QRS complex in lead I and negative QRS complex in leads II and aVF).
The two causes for an extremely leftward axis are an old inferior wall myocardial infarction with deep Q waves in leads II and aVF or a left anterior fascicular block with an rS morphology in leads II and aVF; this is left anterior fascicular block.
There is an R′ waveform in leads V1-V2 (←) associated with a normal QRS complex duration; this indicates a right ventricular conduction delay, which is a normal variant. The QT/QTc intervals are prolonged (360/480 msec), possibly as a result of drug therapy.
Multifocal Atrial Tachycardia (MAT)
Multifocal atrial tachycardia is often seen in association with pulmonary disease, including pulmonary hypertension, as well as heart failure. Multifocal atrial tachycardia may occasionally revert to atrial fibrillation.
Initial therapy is directed at controlling symptoms, which are usually the result of a rapid ventricular response rate. Hence AV nodal blocking agents are useful for symptom relief.
Treatment of the arrhythmia itself is more challenging. The first approach is to treat the associated underlying medical condition. There is some evidence of benefit for potassium or magnesium replacement if either hypokalemia or hypomagnesemia is present. Data regarding the efficacy of verapamil or b-blockers are limited. The standard anti-arrhythmic agents are not of proven benefit.