ECG Intepretation
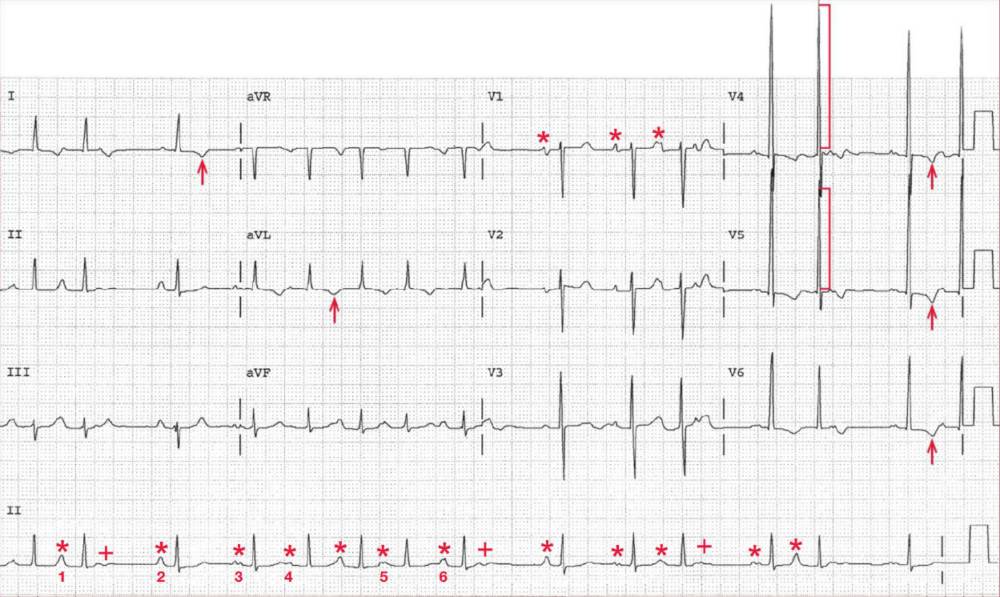
The rhythm is irregularly irregular at an average rate of 90 bpm. There is a P wave (*) before each QRS complex; some P waves after the QRS complexes are nonconducted (+).
There are more than three different P-wave morphologies (1-6) and PR intervals. No one P-wave morphology is dominant. This is termed wandering atrial pacemaker or multifocal atrial rhythm.
This arrhythmia is commonly seen in patients with chronic lung disease. When the rate exceeds 100 bpm, this is termed multifocal atrial tachycardia. It is one of three supraventricular rhythms that are irregularly irregular, the other two being atrial fibrillation and sinus arrhythmia.
The QRS complex has a normal duration (0.08 sec) and a normal axis, between 0° and +90° (positive QRS complex in leads I and aVF). The QT/QTc intervals are normal (360/440 msec).
The QRS complex amplitude in leads V4-V5 is very high (30 mm) ( ] ), consistent with left ventricular hypertrophy. Associated with the hypertrophy are ST-T wave changes (f) in leads I, aVL, and V4-V6.
What is Wandering Atrial Pacemaker (Multifocal Atrial Rhythm) ?
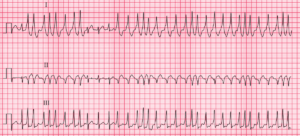
Wandering atrial pacemaker (rate < 100 bpm) or multifocal atrial tachycardia (rate > 100 bpm) is identified by the presence of a distinct P wave before each QRS complex and more than three different P-wave morphologies, without any one P-wave morphology being dominant. PR intervals are variable, and hence the PP and RR intervals are irregularly irregular.
This arrhythmia is most commonly associated with pulmonary disease, especially when there is respiratory decompensation. Wandering atrial pacemaker (multifocal atrial rhythm) can occur in the presence of coronary, valvular, hypertensive, and other types of heart disease, particularly when associated with heart failure and pulmonary congestion or underlying lung disease.
The arrhythmia often resolves spontaneously when the underlying pulmonary or cardiac problem is corrected. On occasion these arrhythmias may degenerate into atrial fibrillation. The changing morphology of the P waves and the PR interval has suggested that the pacemaker arises in different atrial locations.
Generally, no therapy is necessary for the arrhythmia itself. Rather, therapy should be directed at the underlying medical condition. If the ventricular rate is rapid, it can be slowed by blocking the AV node with a calcium-channel blocker.
A beta-blocker is often contraindicated if there is an underlying pulmonary problem, particularly in the presence of wheezing.
There is some evidence that in the presence of hypomagnesemia or hypokalemia, magnesium or potassium replacement may be of benefit for reverting this arrhythmia.