The ECG shows a regular rhythm at a rate of 120 bpm. There is a P wave (*) before each QRS complex, with a stable PR interval (0.14 sec). The P wave is upright in leads I, II, aVF, and V4-V6, and the P-wave morphology is normal. This is sinus tachycardia.
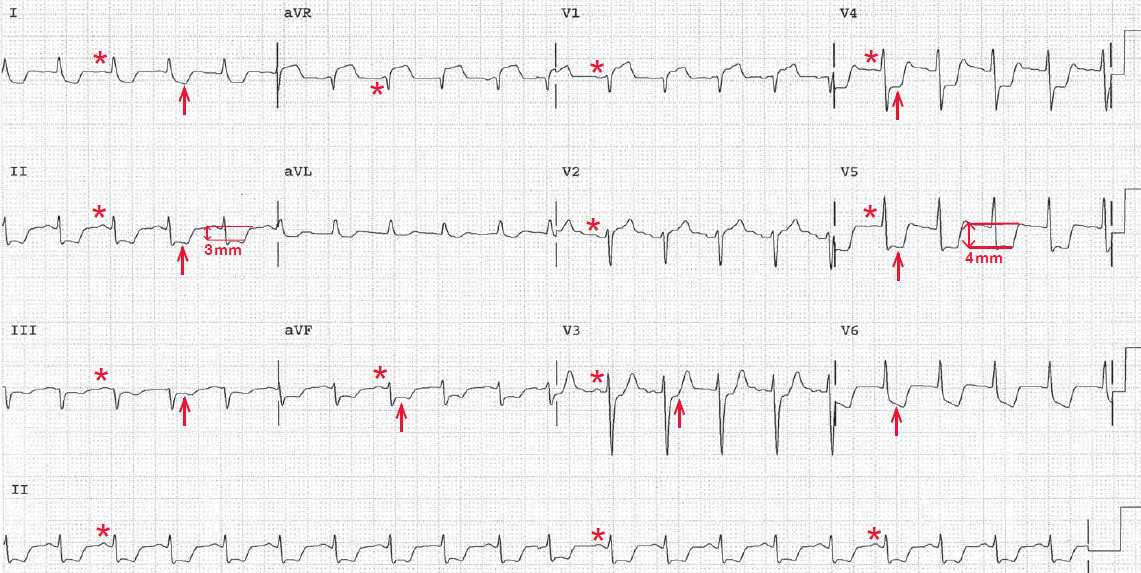
Diffuse J-point and ST-segment depression (↑) can be seen in almost all leads. The ST segments are 3 to 4 mm below the baseline (TP segment) (↕) and are horizontal, except in leads I and V6, where the ST-segment depression is downsloping. Horizontal ST-segment depression is more specific for ischemia than upsloping ST-segment depression.
There is ST Segment elevation in lead V1 and aVR. The ST elevation in lead aVR is reciprocal to the diffuse ST depression.
Diffuse ST depression which is maximal in V4-V6, MUST come with reciprocal STE in aVR, and this represents diffuse supply/demand mismatch (Diffuse Subendocardial Ischemia), for which the differential is enormous. It includes tachycardia, severe anemia, septicemia, hypoxemia, shock, serious arrhythmias, cardiac arrest, “sick patient”, and significant underlying coronary disease (Multivessel Coronary Disease, Proximal LAD or Left Main Artery Disease).
Although the leads in which ST-segment depression is seen do not necessarily correlate with the location of ischemia, the finding of widespread ST-segment depression does correlate with significant, probably multivessel coronary artery disease.
The degree of ST-segment depression (ie, number of millimeters depressed) also correlates with the severity of the coronary disease. This patient likely has multivessel coronary disease.
Although her chest discomfort is atypical for ischemia, she is both diabetic and female. In both of these situations ischemic chest discomfort may present with atypical features. Therefore, additional anti-ischemic therapy should be initiated (ie, a long-acting nitrate and increased dose of β-blocker to further reduce her heart rate with activity).
If symptoms persist, further delineation of the coronary anatomy is warranted. This is usually accomplished with diagnostic coronary angiography. If multivessel disease is confirmed, this patient will likely require revascularization, either with a percutaneous intervention or coronary artery bypass graft surgery.
In most cases, symptomatic ischemia in the presence of diabetes mellitus and multivessel disease, particularly involving the left main or left anterior descending artery, is an indication for surgical revascularization.