This article is an answer and interpretation of the: ECG Case 152
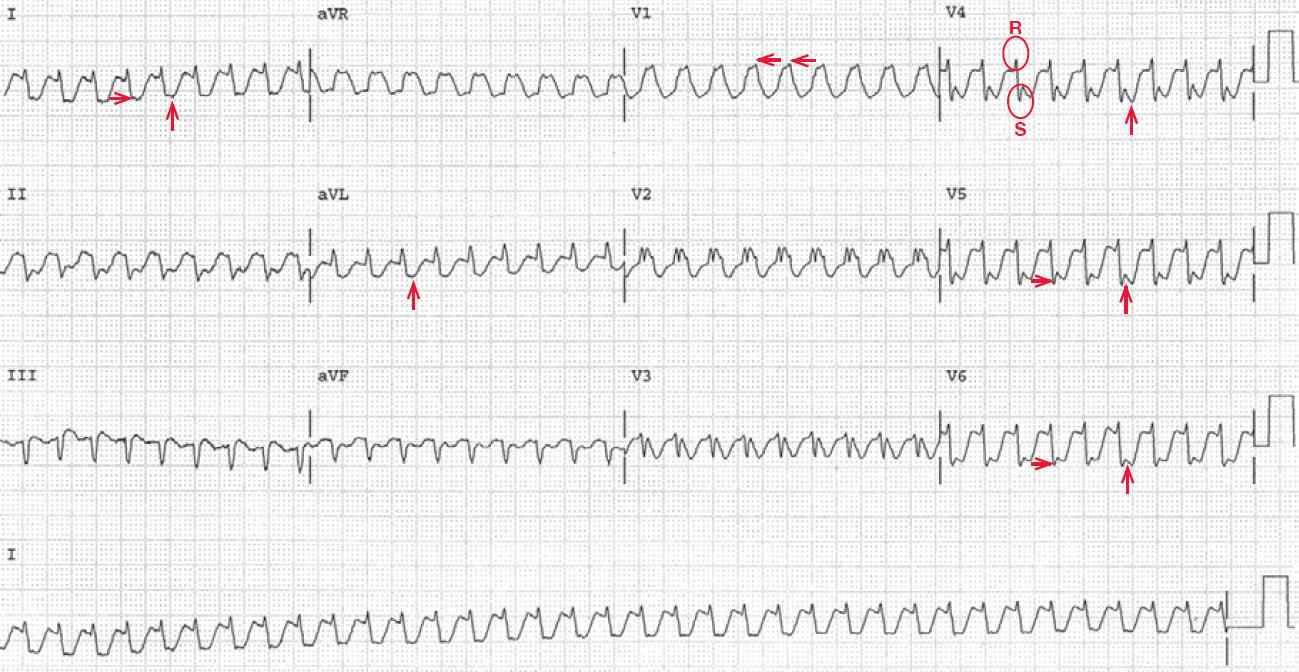
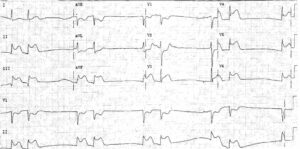
ECG 1 shows a regular rhythm at a rate of 220bpm. There are no P waves seen before or after any QRS complex. The QRS complex duration is increased (0.16sec) and there is a right bundle branch block morphology (broad R wave in lead V1 [←] and broad S waves in leads I and V4–V6 [→]).
Noted is that the initial R wave in leads V4–V6 is narrow (<100msec) while the S wave is widened and accounts for the increase in the QRS duration. Hence this is a criterion for a supraventricular tachycardia with a right bundle branch block. In addition, the axis is extremely leftward between –30° and –90° (positive QRS complex in lead I and negative in leads II and aVF).
The two etiologies for an extreme left axis are an inferior wall myocardial infarction, in which there is a deep initial Q wave in leads II and aVF, or a left anterior fascicular block, in which there is an rS QRS morphology in leads II and aVF. Therefore, this is a left anterior fascicular block.
There is possible ST-segment depression seen in leads I, aVL, and V4–V6 (↑), although it is not clear where the S wave ends and the ST segment begins. Noted is low voltage, defined as a QRS complex amplitude <5 mm (little boxes) in each limb leadand/or <10 mm in each precordial lead.
With the absence of Pwaves, this is termed a no-RP tachycardia. The absence of atrial activity and the rate of 220 bpm of the supraventricular rhythm makes the most likely etiology a typical atrioventricular reentrant tachycardia (AVNRT).
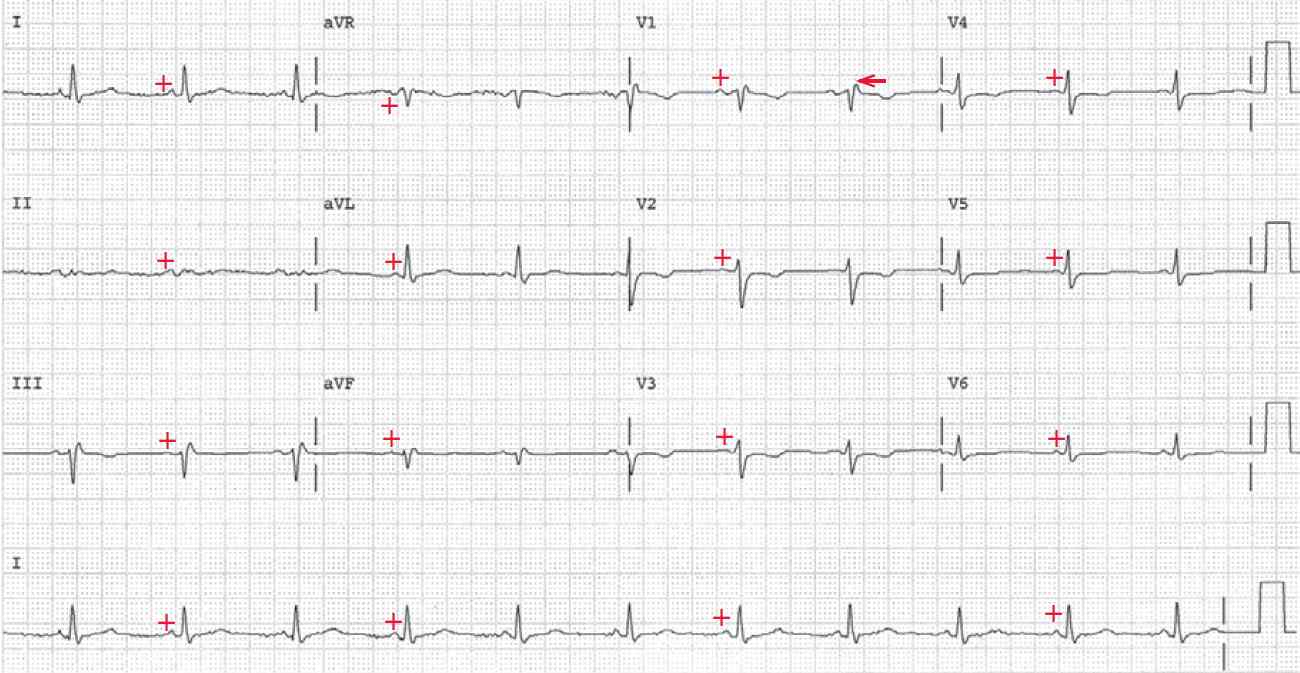
ECG 2 is from the same patient. There is a regular rhythm at a rate of 66bpm. There is a P wave (+) before each QRS complex with a stable PR interval (0.16sec). The P wave is positive in leads I, II, aVF, and V4–V6; hence this is a normal sinus rhythm.
The QRS complex duration is normal (0.10sec) and there is an R′ in lead V1 (←), which is the result of an intraventricular conduction delay to the right ventricle. The axis is leftward between 0° and –30° (positive QRS complex in leads I and II and negative in lead aVF). The QT/QTc intervals are normal (410/430msec).
There is diffuse low voltage (QRS complex <5mm or little boxes in each limb lead and <10mm in each precordial lead). The right bundle branch block morphology is no longer present as the rate is slow. This confirms the fact that ECG 1 showed an AVNRT with a rate-related right bundle branch block aberration.
An AVNRT can be terminated whenever there are changes of conduction of either the slow or the fast pathway, although the slow pathway is usually the limb that is affected. Changes in the electrophysiologic properties can be produced by changing autonomic tone, for example, a vagal maneuver such as Valsalva or carotid sinus pressure will slow or block impulse conduction.
Adenosine can also slow or block AV nodal conduction is an effective therapy for terminating this arrhythmia. AV nodal blocking agents such a b-blockers, calcium-channel blockers (verapamil or diltiazem), or digoxin are also effective.
- READ ALSO:
- SIMILAR CASES: