A 70-year-old woman with end-stage liver disease from hepatitis C was admitted to the hospital for confusion. Portosystemic encephalopathy was diagnosed, and the patient was treated with 20 g of lactulose every 6 hours.
A few days after admission, abdominal pain with marked abdominal distention developed. There was no fever or leukocytosis.
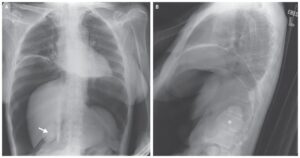
Abdominal radiography showed a distended, air-filled colon to the level of the splenic flexure, with the cecum and transverse colon measuring 11 cm and 14 cm, respectively.
Subsequent abdominal computed tomography showed marked distention of the proximal colon with an abrupt transition to a decompressed colon at the level of the proximal descending colon, with no evidence of an obstructing lesion.
A diagnosis of acute colonic pseudo-obstruction, or Ogilvie’s syndrome, was made. She was initially treated conservatively with the administration of intravenous fluids and the use of nasogastric and rectal tubes. The use of neostigmine was contraindicated, given the acute renal failure.
When her abdominal discomfort worsened, colonoscopic decompression was performed, resulting in marked improvement.
Acute colonic pseudo-obstruction is characterized by massively dilated large-bowel segments in the absence of mechanical obstruction and can be seen in a wide variety of medical and surgical illnesses.