This article is an answer to the Case – Cough with Purulent Sputum, Dyspnea and Haemoptysis
On this admission examination revealed tachycardia with pulse of 120/ min. and regular, pyrexia of 38 degree C, hypoxia with oxygen saturation of 89 % on air, respiratory rate 30 / minute and blood pressure 120/75 mm Hg. Respiratory system examination showed stony dullness and absent air entry in left hemithorax.
Inflammatory markers were raised – white cell count 20.5 *109/l (neutrophils 17.9 *109/l), CRP 311 mg/l on routine blood examination. Urea and electrolytes were normal. Arterial blood gas FiO2 35 % – pH 7.39, pCO2 -5.46, pO2 -13.32, HCO3 -24.6, base excess -0.2.
Imaging Findings
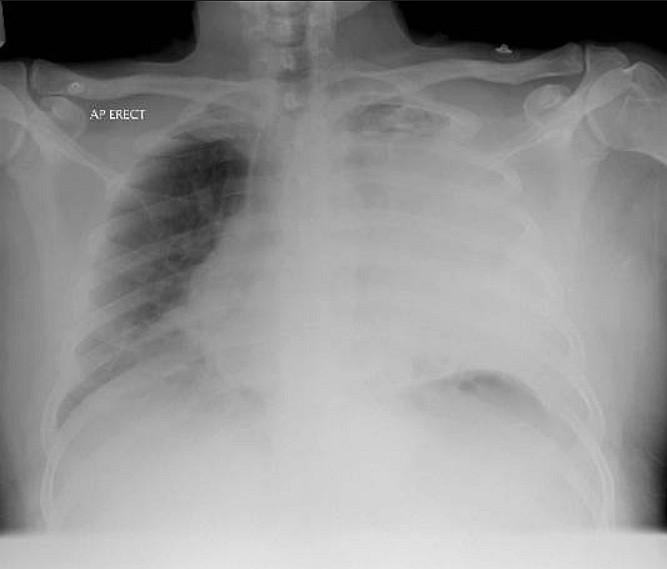
CXR revealed complete white out of left hemithorax and mediastinal shift to opposite side raising the possibility of massive pleural effusion or empyema. CT thorax revealed left pyopneumothorax.
Patient was treated initially with left intercostal drain, intravenous antibiotics and then had a limited decortication and was to be considered for lobectomy at a later stage.
Discussion
Bronchiectasis has been defined as the abnormal and permanent dilatation and distortion of conducting bronchi and airway. Bronchiectasis is categorized in the spectrum of chronic obstructive pulmonary disease (COPD); it is characterized by inflamed airways which collapse easily resulting in the air outflow obstruction and impaired clearance of the secretions. Its prevalence increases with age and it is more common in females.
This damage can be congenital or may be acquired. Various factors like cigarette smoking, foreign body aspiration, rheumatic disease etc. all contribute to the damage. Usual clinical manifestations include cough, dyspnoea, wheezing and daily production of mucopurelent sputum, lasting for months to years and frequent visits to the hospital with repeated courses of antibiotic treatments. Patients with bronchiectasis have a longer duration of symptoms during exacerbations of COPD, a greater burden of pathogenic bacterial pathogens in the lower airway, and increased sputum inflammatory markers but the frequency of attacks is not increased.
CXR Findings in Bronchiectasis
CXR is abnormal in 90% of cases. Abnormal findings include increased bronchovascular markings from peribronchial fibrosis and intrabronchial secretions, tram lines (parallel lines outlining dilated bronchi due to peribronchial inflammation and fibrosis), honeycombing, cystic areas with or without fluid levels and rib crowding from an atelectatic lung.
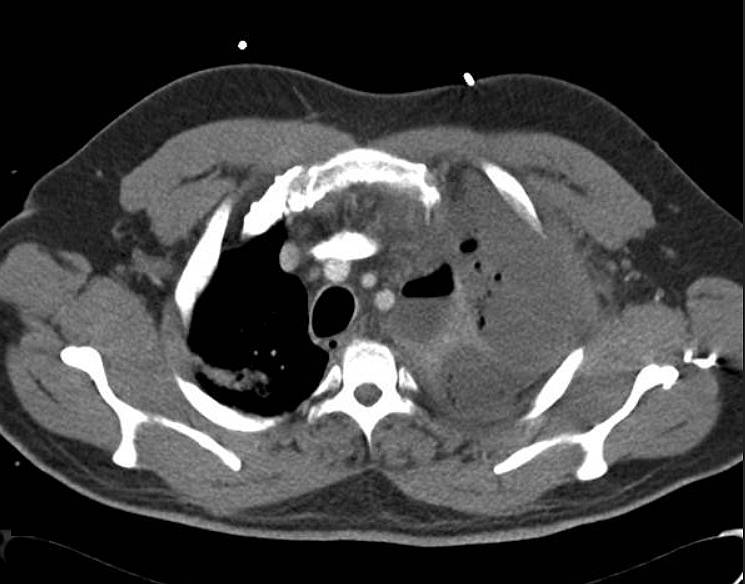
High Resolution Computed Tomography (HRCT) Findings
High Resolution Computed Tomography (HRCT) is the gold standard test with sensitivity of 97%. Specific abnormality seen is dilation of airway more than 1.5 times the normal diameter. HRCT also shows ‘signet ring’ sign which is cross-sectional appearance of dialated bronchus abutting the pulmonary artery.
Non specific abnormalities include airway dilation, bronchial wall thickening, plugging of airways by mucus, cysts indicating destructive disease. Other HRCT findings are lack of bronchial tapering, visualizing of bronchi within 1cm of costal pleura and adjacent to mediastinal pleura.
References
- Bronchiectasis, exacerbation indices, and inflammation in chronic obstructive pulmonary disease. AU Patel IS; Vlahos I; Wilkinson TM; Lloyd-Owen SJ; Donaldson GC; Wilks M; Reznek RH; Wedzicha JA SO Am J Respir Crit Care Med 2004 Aug 15;170(4):400-7. Epub 2004 May 6. (PMID: 15130905)
- Desai SR, Wells AU, Cheah FK, Cole PJ, Hansell DM. The reproducibility of bronchial circumference measurements using computed tomography. Br J Radiol 1994;67:257-262. (PMID: 8130998)
- Ouellette H. The signet ring sign. Radiology. 1999 Jul;212(1):67-8. (PMID: 10405722)
- Pryor JA. Physiotherapy for airway clearance in adults. Eur Respir J 1999;14:1418-1424. (PMID: 10624775)
- Agasthian T, Deschamps C, Trastek VF, Allen MS, Pairolero PC. Surgical management of bronchiectasis. Ann Thorac Surg 1996;62:976-980. (PMID: 8823075)
- Kumar NA, Nguyen B, Maki D. Bronchiectasis: current clinical and imaging concepts. Semin Roentgenol. 2001 Jan;36(1):41-50. (PMID: 11204758)
- Hansell DM. Bronchiectasis. Radiol Clin North Am. 1998 Jan;36(1):107-28. (PMID: 9465870)