This post is an answer to the Case – Facial Flushing
What is this syndrome, and what is the origin of the tumour that produces it?
The carcinoid syndrome. The primary tumour arises in the Kultschitzky cells* of the intestinal mucosal crypts, which characteristically take up silver stains.
What is the commonest site of the tumour?
The majority are found in the appendix and are found incidentally at laparotomy or present as acute appendicitis. The great majority of these are relatively benign and do not recur after a simple appendicectomy. However, a small percentage, about 4%, develop secondary spread.
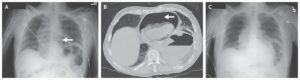
More rarely, carcinoid tumours are found in the distal ileum or proximal large bowel, and these typically spread to the regional nodes and to the liver, as in the case of this patient. Rarely they occur in the lung. About 10% are associated with the multiple endocrine neoplasia type 1 (MEN-1) syndrome.
What other clinical features may be found in the carcinoid syndrome?
As well as the enlarged liver and flushing with attacks of cyanosis, there may be diarrhoea with abdominal pain and noisy borborygmi, bronchospasm and pulmonary and tricuspid valve stenosis.
What is the biochemical basis of these features?
The carcinoid tumour secretes 5-hydroxytryptamine (5- HT, also known as serotonin), in addition to a variety of other hormones. The liver is normally able to inactivate these hormones as they reach this organ via the portal vein. However, in the presence of liver metastases, 5-HT is secreted directly into the systemic circulation, with the appearance of the above effects.
What biochemical investigation is used to clinch the diagnosis?
5-HT is excreted in the urine as 5-hydroxyindole acetic acid (5-HIAA). A raised level of this is found in a 24h urine collection from the patient.
What modalities of treatment are available?
It may be possible to resect the liver metastases if these are not too extensive. If widespread, the deposits can be embolized via a catheter introduced into the femoral artery and guided into the hepatic artery. This was indeed carried out in this patient with a gratifying remission. In other cases, cytotoxic drugs may be used.
Symptoms may be controlled using 5-HT antagonists, e.g. methysergide or octreotide, the latter being a somatostatin analogue that inhibits the release of 5-HT. Even if widespread deposits are present, it is well worthwhile persevering with treatment as the tumour is slow growing and the patient may survive for many years in reasonable health.