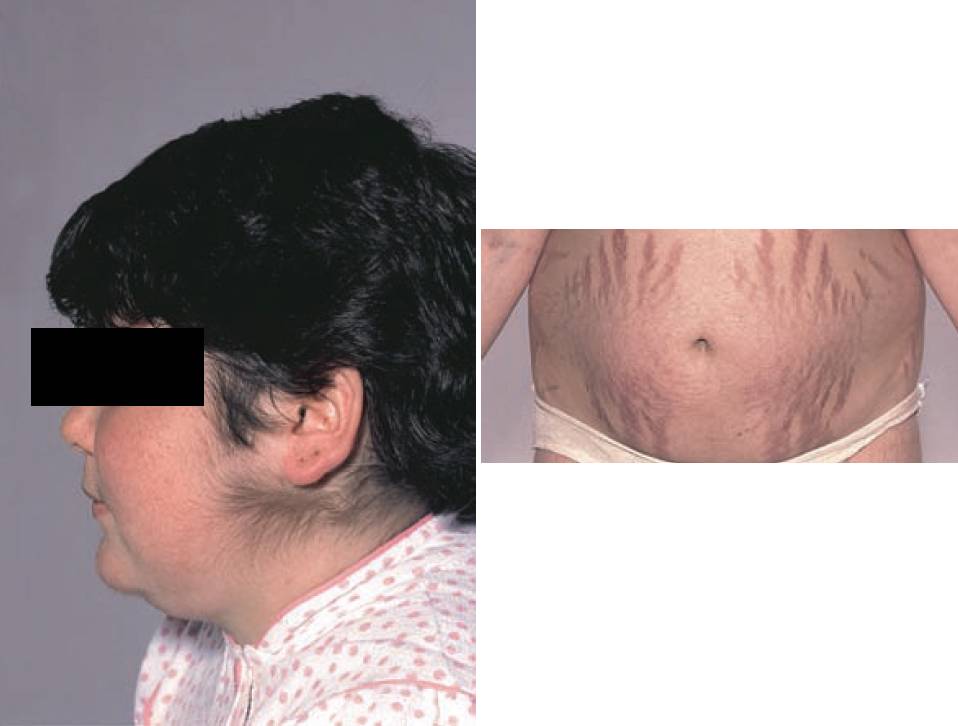
This post is an answer to the Case – Female with Excessive Hair on Face and Abdominal Striae
What is the eponymous name of the endocrine disease from which she is suffering?
Cushing’s syndrome.
What are the possible causes of this condition?
Cushing’s syndrome occurs when there is prolonged exposure to supraphysiological levels of circulating glucocorticoids. The etiology of Cushing’s syndrome is most easily considered in terms of whether it is adrenocorticotrophic hormone (ACTH) dependent or independent:
- ACTH-dependent Cushing’s syndrome:
- Pituitary adenoma (so-called Cushing’s disease).
- Ectopic ACTH secretion (e.g. from a small cell carcinoma of the lung).
- ACTH-independent Cushing’s syndrome:
- Exogenous steroids.
- Suprarenal adenoma or carcinoma.
Most important effects of oversecretion of suprarenal corticosteroids.
- Obesity: Principally involving the trunk and neck – so-called centripetal.
- Skin changes: Hirsutism, abdominal striae, excessive bruising, thin skin.
- Raised blood pressure.
- Proximal muscle weakness/wasting: Especially of the shoulder and pelvic girdles.
- Glucose intolerance/diabetes mellitus.
- Mental disturbance: Depression or psychosis.
- Growth retardation in childhood.
What laboratory and imaging investigations are useful in such cases?
The investigation of Cushing’s syndrome should be considered in two stages.
- Confirmation of hypercortisolism: Typically two or more of the following tests are used to confi rm the diagnosis:
- Elevated 24 h urinary free cortisol (UFC) excretion – a minimum of three collections are required to ensure that mild cases are not missed.
- Failure of cortisol to suppress in response to dexamethasone. An overnight test administering 1 mg dexamethasone is often used for screening purposes, but has a significant false-positive rate, hence the conventional low dose 48 h test (0.5 mg 6-hourly for 48 h) should be used to confirm the diagnosis.
- Loss of circadian rhythm, with elevated midnight cortisol levels.
- Identification of source: Measurement of the plasma ACTH helps to differentiate ACTH-dependent from ACTH-independent Cushing’s syndrome.
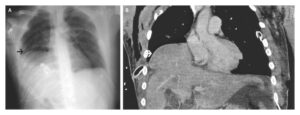
- For ACTH-dependent cases, inferior petrosal venous sinus sampling (IPSS) reliably distinguishes pituitary from ectopic ACTH secretion. Pituitary MR imaging identifies approximately 60% of microadenomas. CT imaging, octreotide scintigraphy and positron emission tomography can be used to help localize ectopic tumours.
- For ACTH-independent cases (low/undetectable levels), a CT scan of the suprarenal glands is the next appropriate investigation.
What treatment is available for patients with Cushing’s syndrome?
In those patients where a suprarenal tumour is found, adrenalectomy is performed. Trans-sphenoidal microsurgery is used to remove a pituitary adenoma. Medical pre-treatment with drugs such as metyrapone and ketoconazole can help to control hypercortisolaemia prior to surgery.
READ MORE: Cushing and Addison’s Disease – Approach, Evaluation and Management
SIMILAR CASE: Primigravid Woman with Proximal Muscle Weakness, Striae, and Facial Plethora