Table of Contents
Cushing’s Syndrome
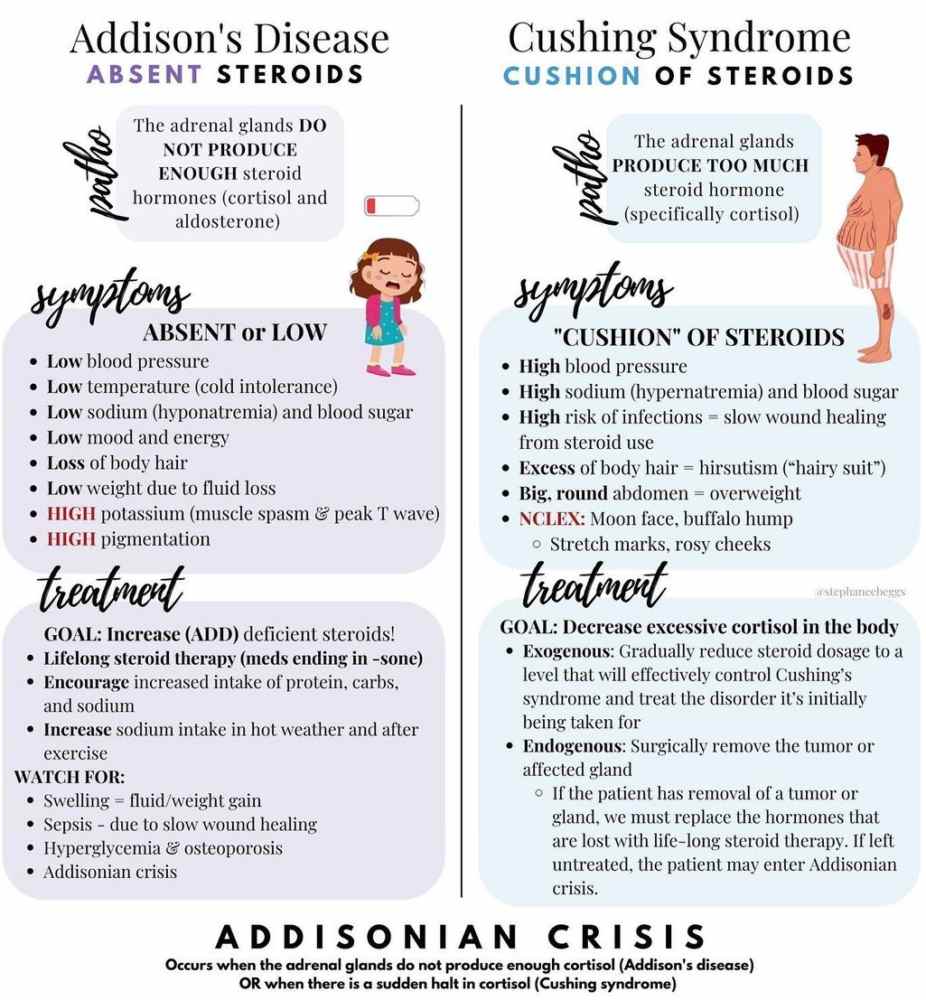
Cushing’s syndrome is the result of chronic exposure to excess glucocorticoid. This is most commonly iatrogenic secondary to glucocorticoid administration given to treat inflammatory diseases. Other causes include the following:
- As a result of ACTH hypersecretion by a pituitary corticotrophic adenoma (60-70%).
- Primary adrenocortical tumors (30%).
- Ectopic ACTH syndrome caused by a variety of ACTH-secreting nonpituitary tumors (5-10%), such as small cell lung carcinoma.
The annual incidence of spontaneous Cushing’s syndrome is about 1 in 100,000, and it is 3-5 times more common in women than men.
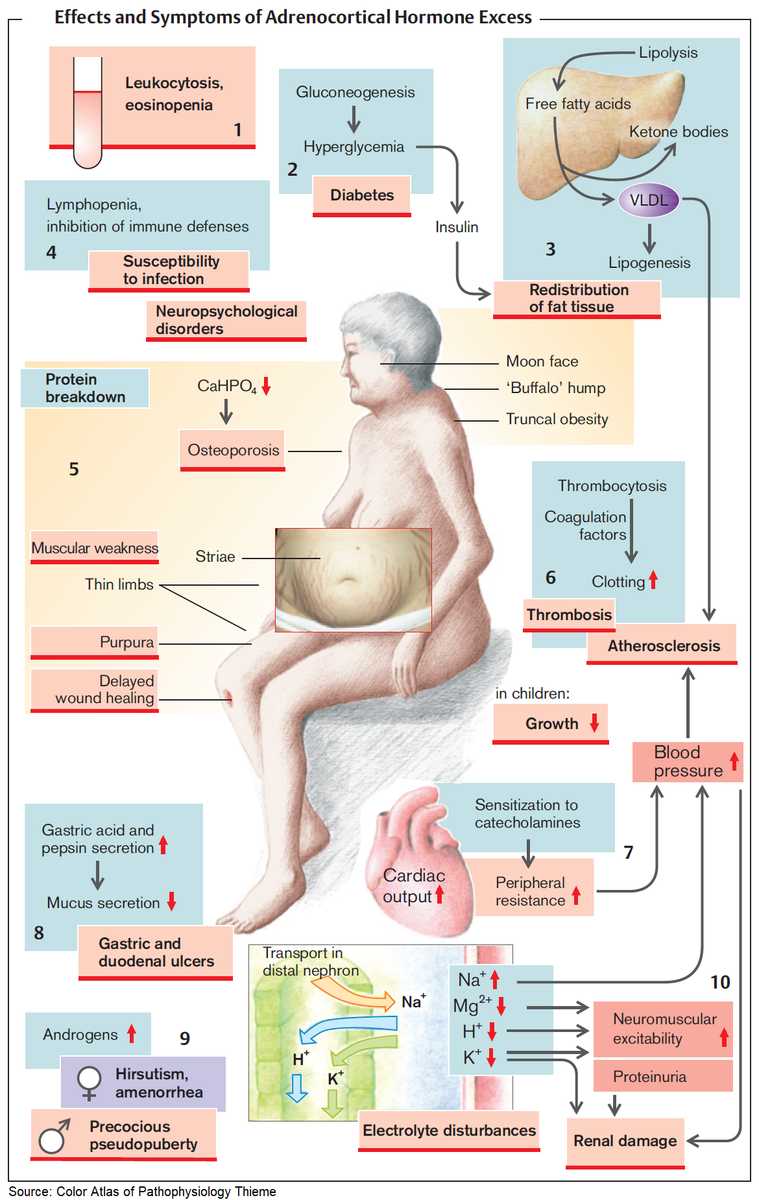
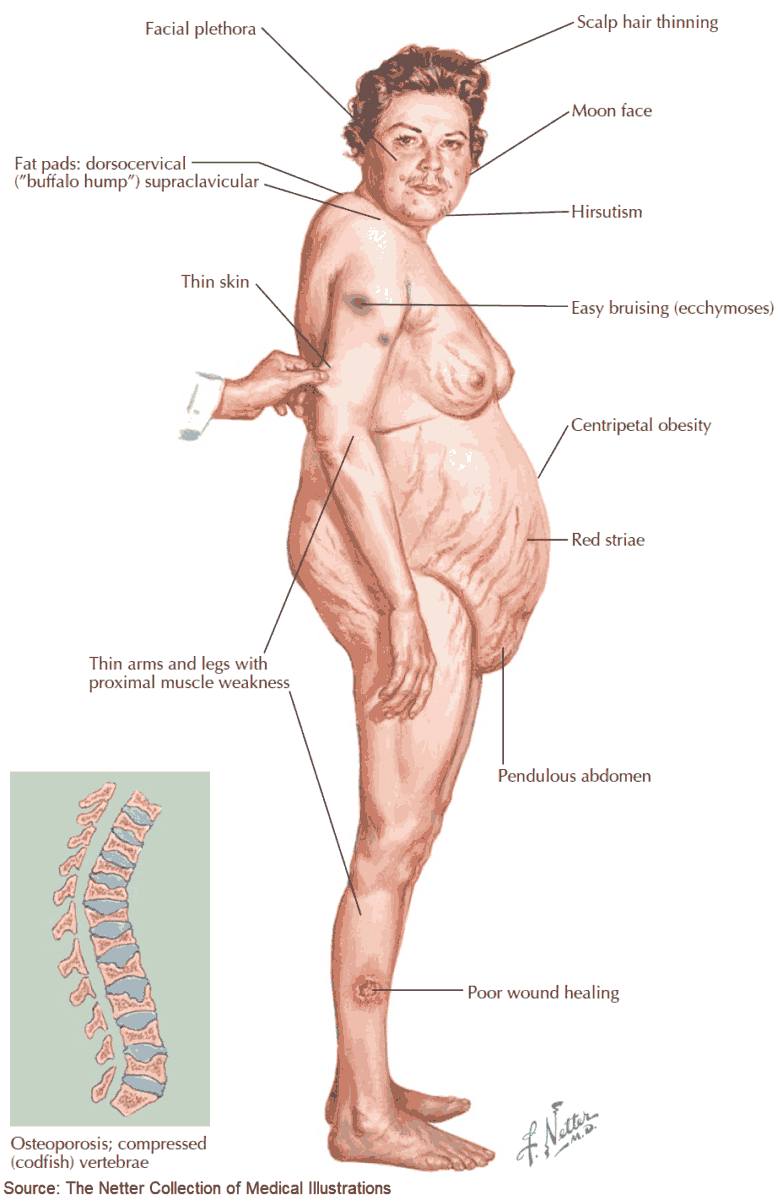
Clinical Features of Cushing’s Syndrome
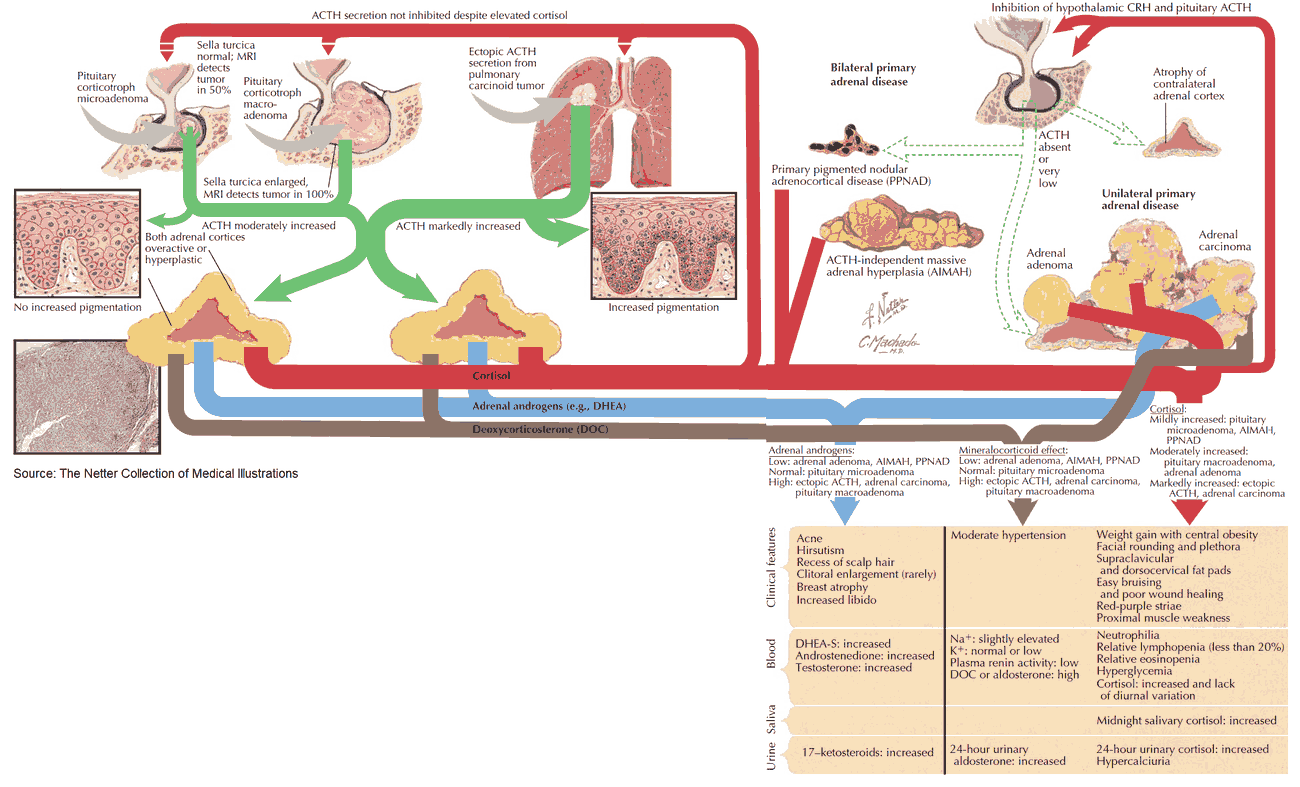
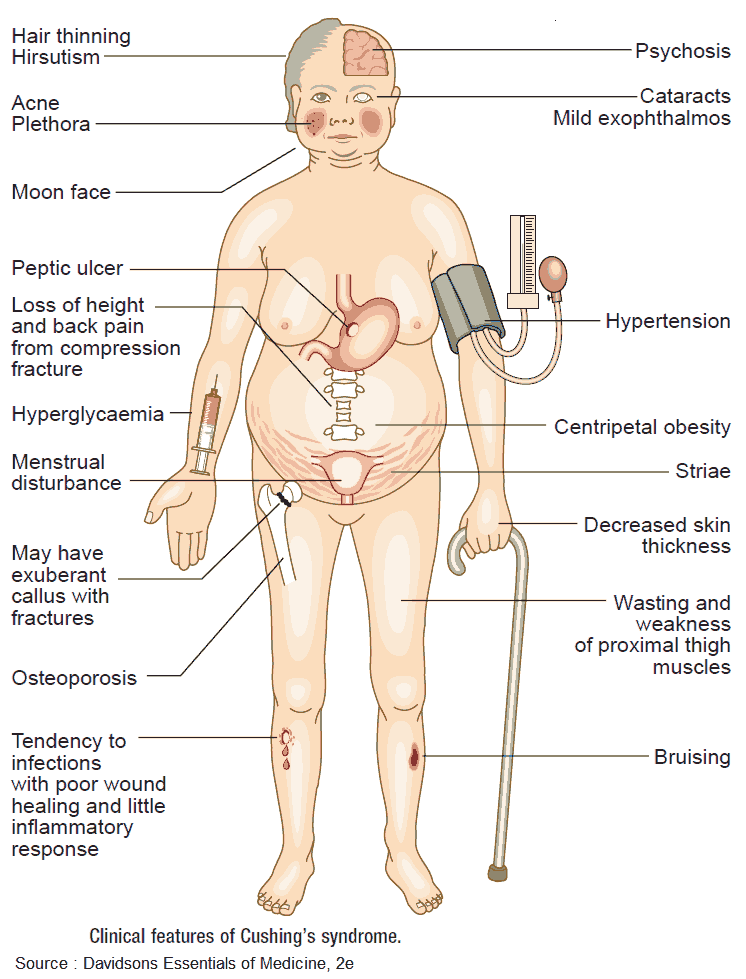
The clinical features of Cushing’s syndrome include the following:
- Centripetal fat deposition producing the typical moon facies and buffalo hump (dorsocervical fat pad).
- Skin thinning, and purple striae over the abdomen and flanks. Bruising is common and wounds heal slowly.
- Lower limb edema.
- Proximal muscle wasting.
- Osteoporosis, particularly of the vertebral bodies, leading to compression fractures.
- Impaired defense against infections.
- Hypertension.
- Mild hirsutism in women.
- Amenorrhea and infertility in women and impotence in men.
- Electrolyte disturbances with hypernatremia and hypokalemia.
- Impaired glucose tolerance or frank diabetes.
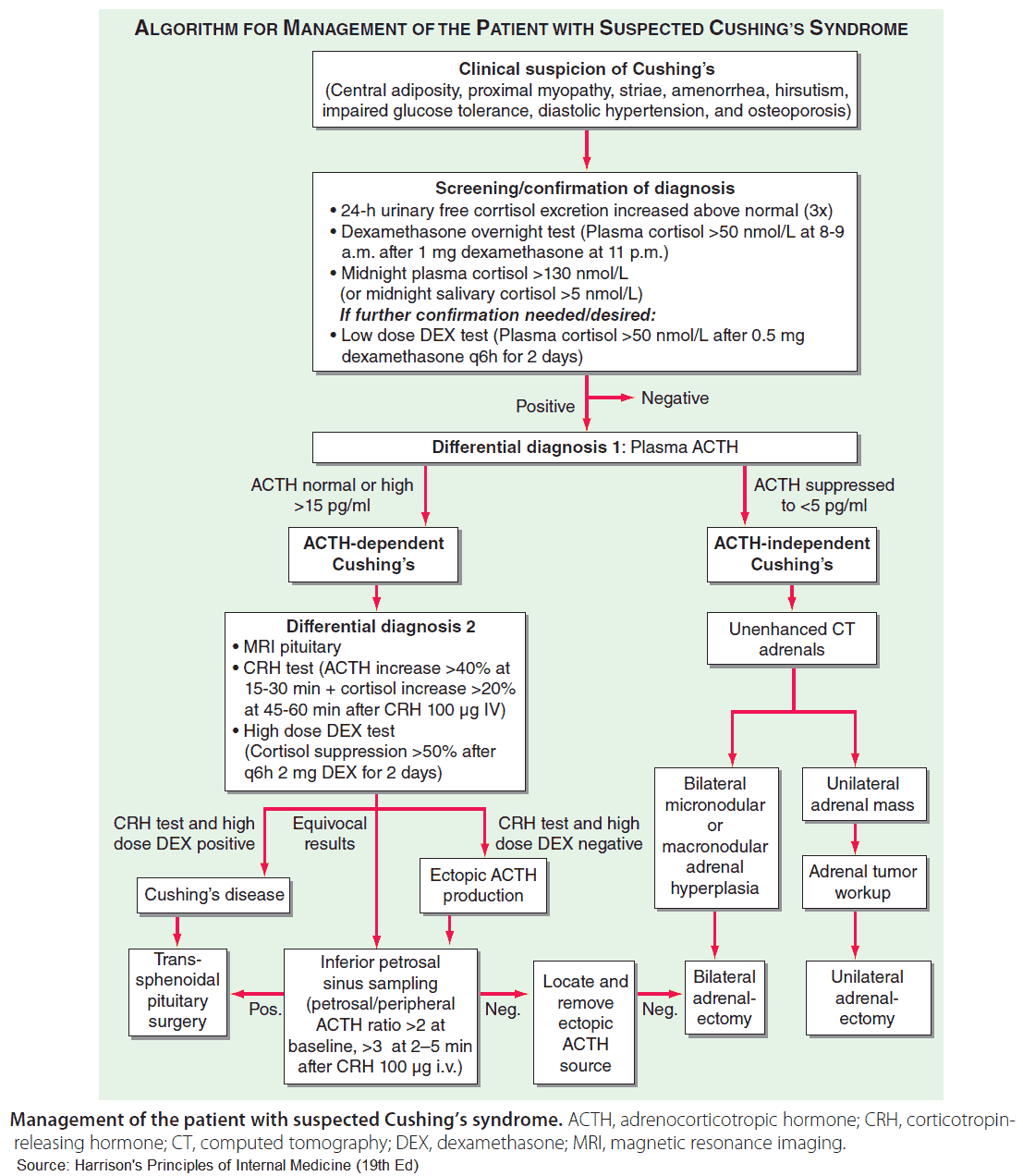
Investigations in Cushing’s Syndrome
Plasma cortisol will vary throughout the day in normal individuals and should be measured at 9 am and 11 pm. Normal circadian rhythm will be lost and levels raised in Cushing’s syndrome. Very low or absent cortisol levels at a time of suspected Addisonian crisis confirms hypoproduction of cortisol.
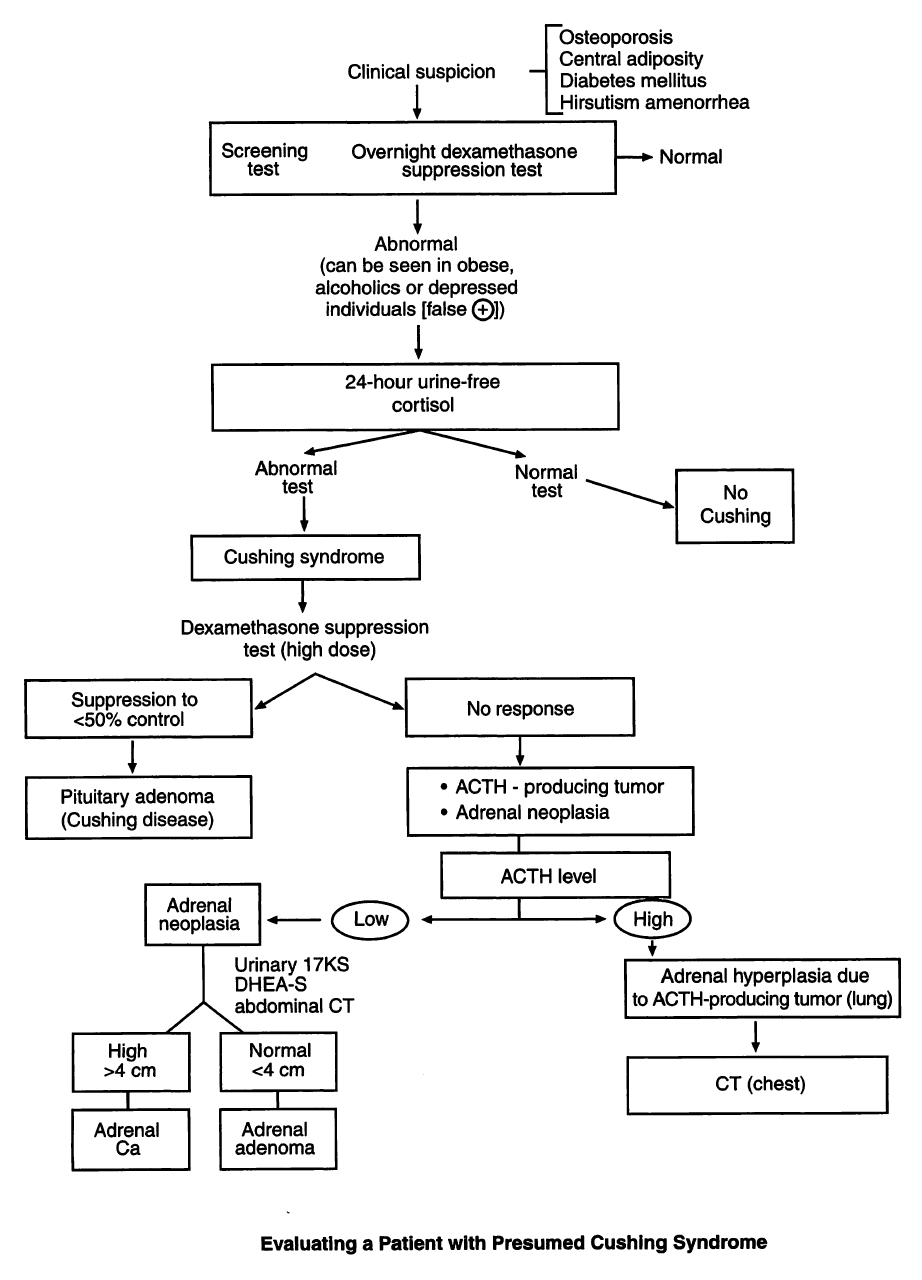
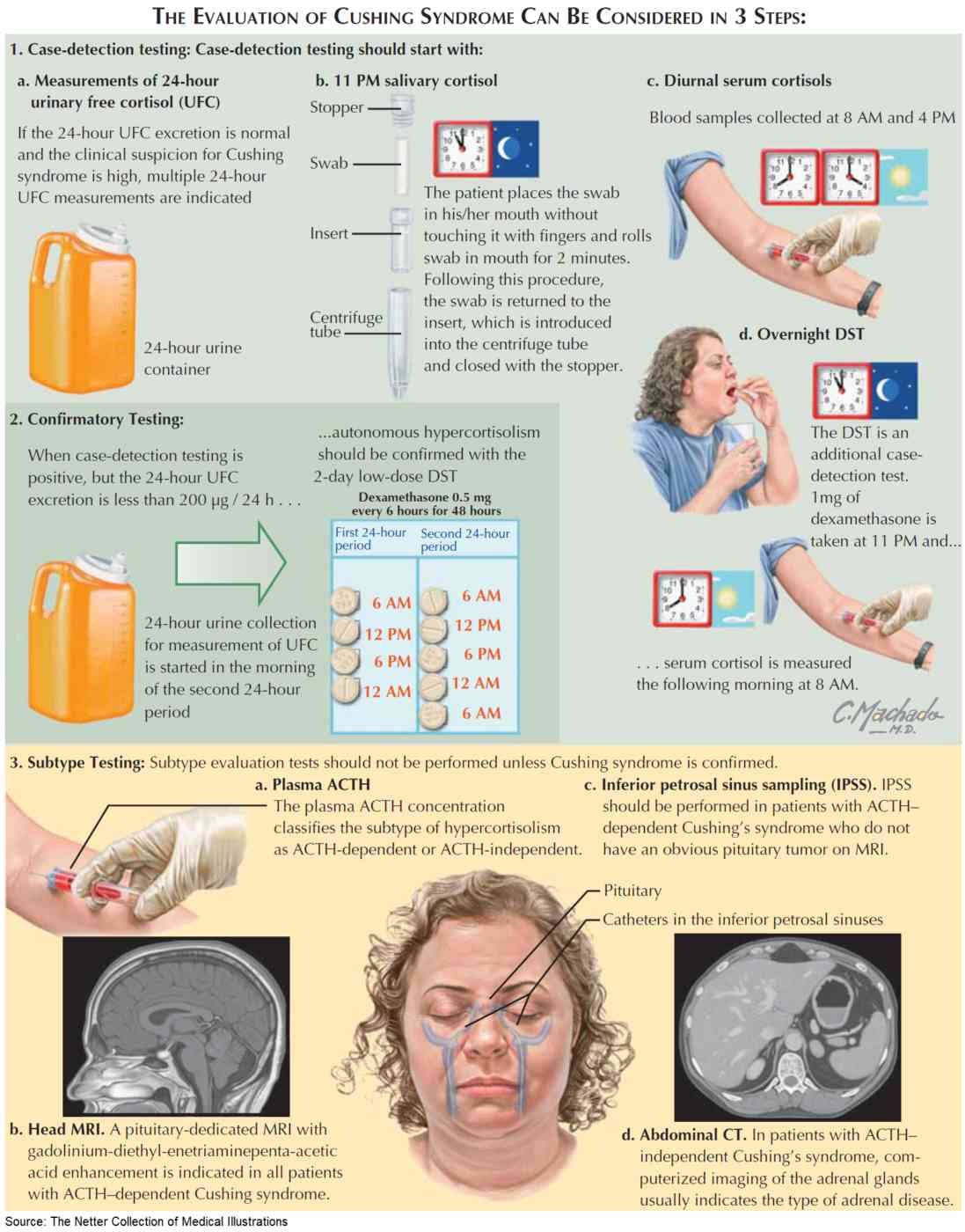
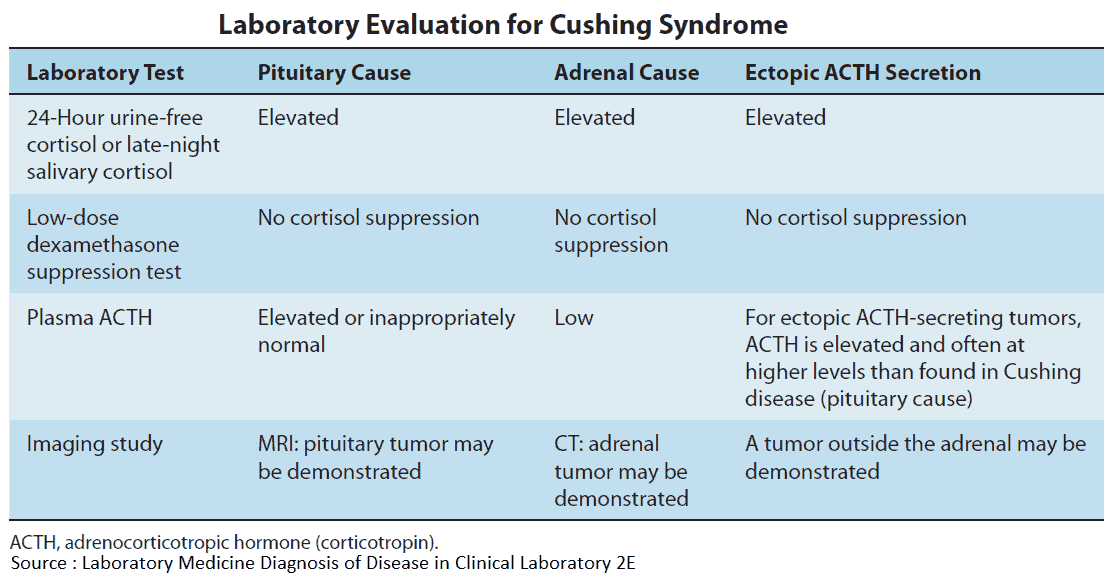
Tests for cortisol excess
Urinary cortisol
A 24-hour estimation of urinary free cortisol is a better predictor of Cushing’s syndrome than plasma cortisol.
Plasma ACTH
This is very high in ectopic ACTH production, moderately raised in Cushing’s syndrome (pituitary adenoma), and very low in adrenal adenoma or carcinoma.
Overnight dexamethasone suppression test
Here, 2 mg oral dexamethasone is taken at 11 pm; plasma cortisol is measured at 9 am the next morning. In normal patients, ACTH and cortisol production will be suppressed by negative feedback, and plasma levels of cortisol will be <5μg/dl (140 nmol/L).
In all cases of Cushing’s syndrome suppression will not occur. In patients with Cushing’s disease the feedback mechanism is less sensitive than normal as ACTH levels are chronically elevated. Ectopic ACTH production has no feedback mechanism; ACTH is always suppressed in those with an adrenal cause.
High-dose dexamethasone suppression test
Plasma cortisol is measured; 2 mg oral dexamethasone is taken every 6 hours for 2 days. After 48 hours from the first dose, plasma cortisol is remeasured. In normal individuals the plasma cortisol should be suppressed to at least half its initial value. This dose of dexamethasone should overcome the less sensitive feedback mechanism in Cushing’s disease but will not cause suppression in ectopic ACTH production and adrenal hyperfunction.
Management
Cushing’s disease
Transsphenoidal surgery is the first line of treatment and is curative in about 80% of patients. Drugs are used if surgery fails. Metyrapone inhibits steroidogenesis and is the drug of choice. Op’DDD has a specific adrenolytic action and is used for patients intolerant to metyrapone.
Rarely, bilateral adrenalectomy is necessary, although this has a risk of leading to Nelson’s syndrome, resulting in hyperpigmentation from excess β-lipotrophin activity (melanocyte-stimulating hormone and ACTH) which is not suppressed by a high blood cortisol.
Adrenocortical tumors
Surgical removal of an adrenocortical tumor is curative. Bilateral adrenalectomy necessitates replacement therapy with cortisol, 20-40 mg daily, and fludrocortisone, 0.1 mg daily.
Ectopic ACTH syndrome
Surgical resection of the tumor cures the hypercortisolism, although this is often not possible.
- READ ALSO:
Addison’s Disease (Adrenal Insufficiency)
Addison’s disease is primary adrenocortical failure. The prevalence is about 100 per million per year, and the incidence is about 5 per 1 million per year.
Causes of Addison’s Disease
Causes of Addison’s disease include the following:
- Autoimmune adrenal destruction: this accounts for up to 90% of cases. Women are affected 2-3 times more often than men. Patients may have other autoimmune endocrine deficiencies.
- Infections: especially tuberculosis; cytomegalovirus and fungal infections associated with AIDS are now becoming common.
- Adrenal hemorrhage/infarction: this may be associated with sepsis, particularly meningococcal septicemia-the Waterhouse-Friderichsen syndrome. The presentation is usually acute.
- Metastatic carcinoma: especially from the breast.
- Inherited disorders: there are several familial disorders of adrenal function, all of which are rare.
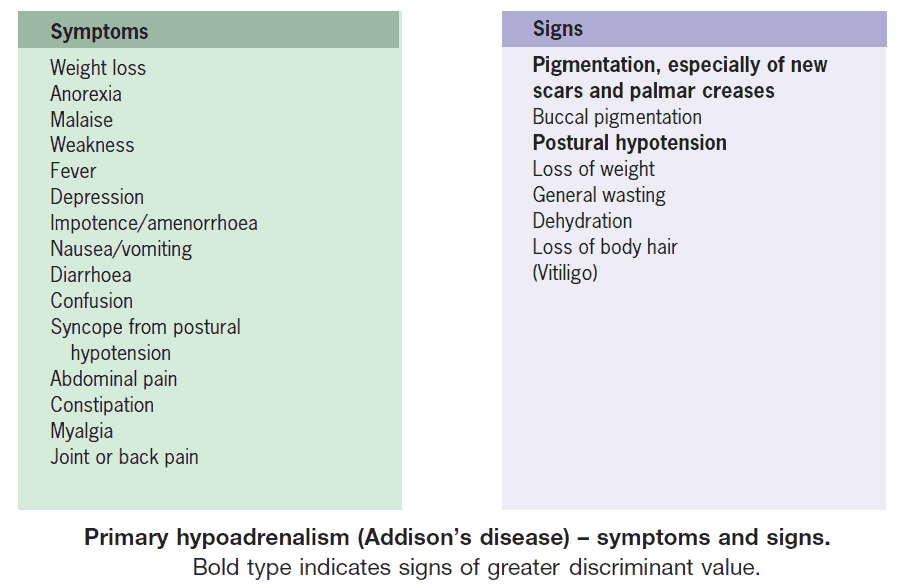
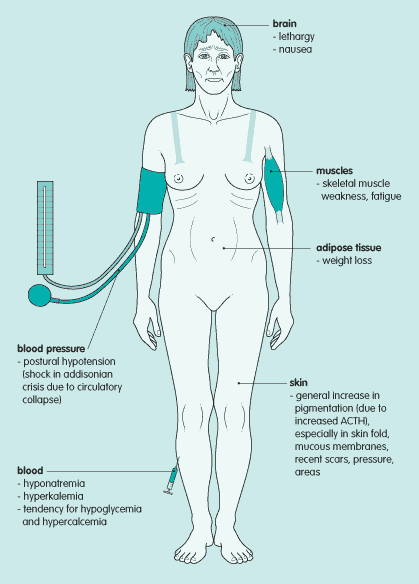
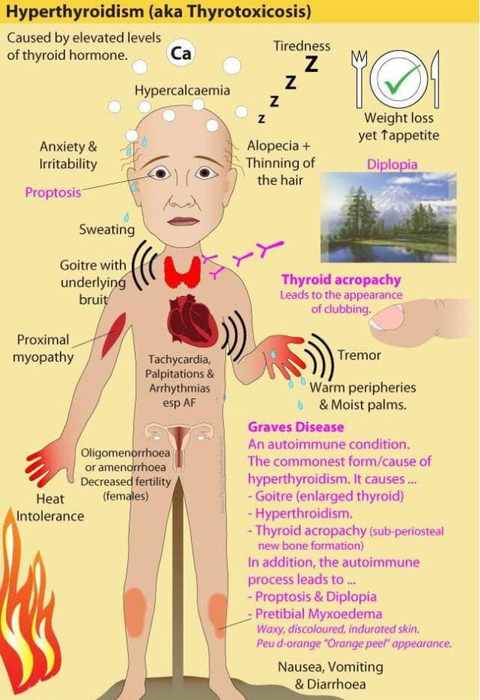
Clinical Features of Addison’s Disease
Symptoms and signs of Addison’s disease are predominantly caused by cortisol deficiency, although deficiencies of aldosterone and adrenal androgen will also be present to varying extents.
The main symptoms are insidious and nonspecific:
- Fatigue,
- Weight loss,
- Orthostatic dizziness, and
- Anorexia.
- GI symptoms (e.g., abdominal pain, nausea, vomiting, and diarrhea).
- Hyperpigmentation of the skin and mucous membranes may occur as a result of high ACTH concentrations.
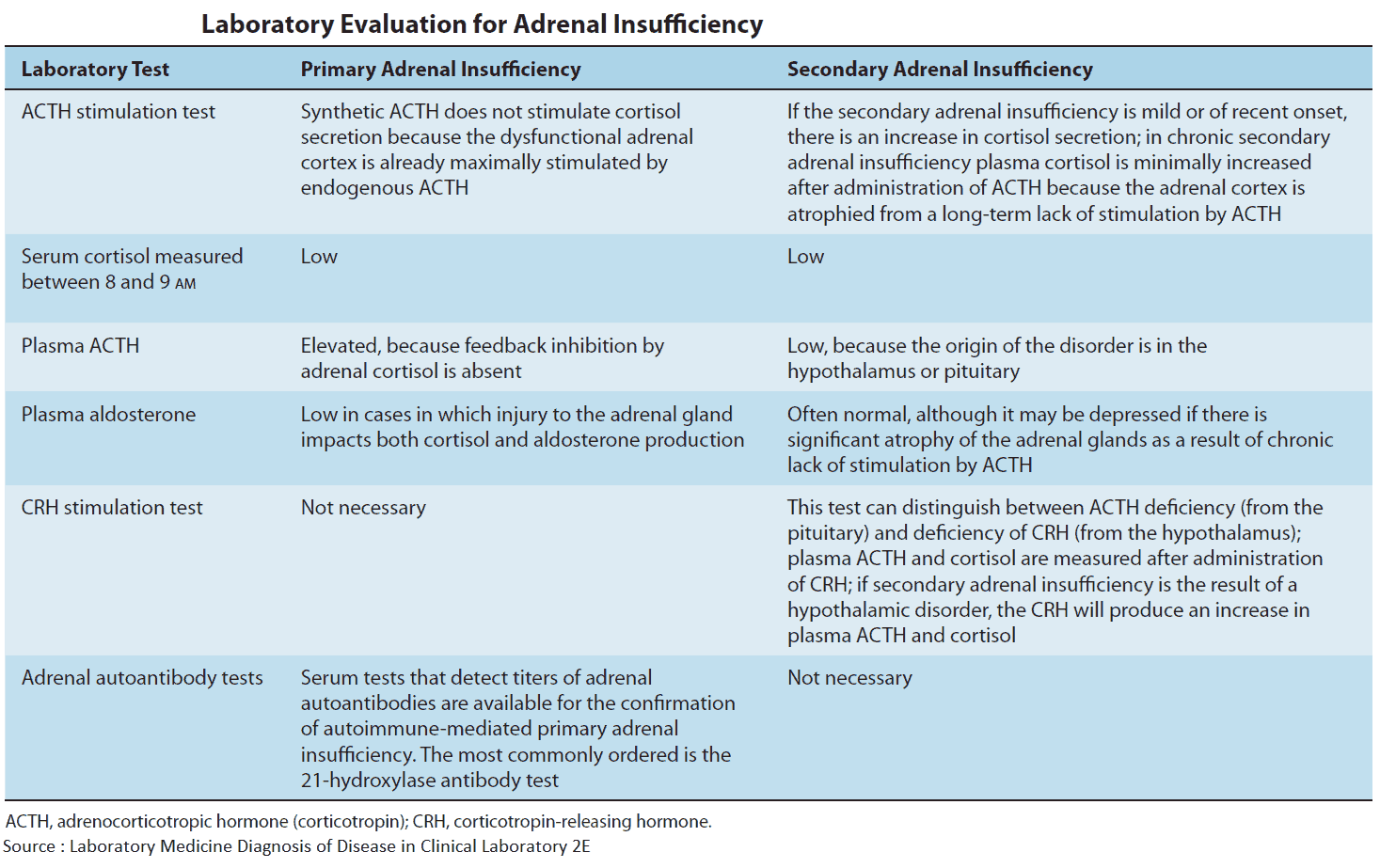
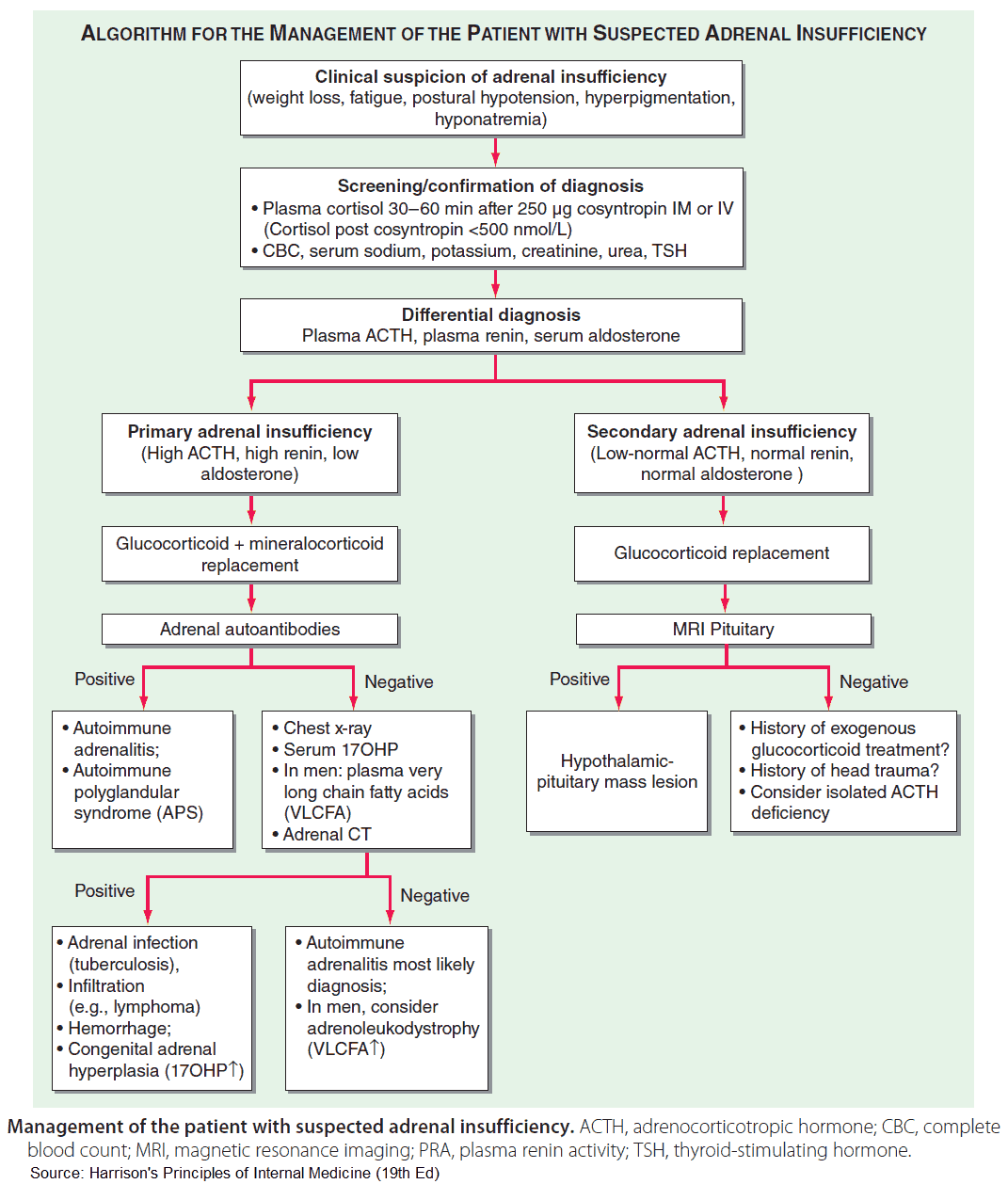
Investigations in Addison’s Disease
The following are important investigations in patient with Addison’s disease:
- Serum cortisol concentration: low.
- Adrenal autoantibodies are detected in about 50% of patients.
- Serum ACTH levels: raised in Addison’s disease and low in secondary failure.
- Serum electrolytes: usually normal but in an impending crisis there may be hyponatremia, hyperkalemia, and raised blood urea.
- Short and long synacthen tests:
- Short ACTH stimulation test: Plasma cortisol is measured (>170 nmol/L normally) and 0.25 mg cosyntropin (synthetic ACTH, which has the same biologic action as ACTH) is given intramuscularly or intravenously. Plasma cortisol is remeasured after 60 minutes. In normal patients, cortisol will rise by a minimum of 190 nmol/L to at least 580 nmol/L. The response will be poor in any case of cortisol hypoproduction.
- Long ACTH stimulation test: Here, 1 mg ACTH is given by intramuscular injection daily for 3 days. Adrenal glands suppressed by the prolonged administration of corticosteroids show a response to this level of stimulation. No response will be seen in adrenal hypofunction
- TFTs: may show low thyroxine and raised TSH.
- Screening for other autoimmune diseases.
Management of Addison’s Disease
In emergencies, intravenous saline and glucose are required. Intravenous hydrocortisone, 100 mg 6 hourly, is given. Underlying infection must be treated.
Maintenance therapy is with hydrocortisone, usually 20 mg in the mornings and 10 mg in the evenings. The dose of hydrocortisone should be increased during intercurrent illnesses and during surgery. Enzyme-inducing drugs (e.g., phenytoin and rifampicin) may also increase patient requirements for hydrocortisone.
Fludrocortisone is used to replace aldosterone because aldosterone taken orally undergoes first pass metabolism through the liver. The dose is adjusted to maintain blood pressure and potassium levels. The usual dose is about 0.1 mg daily.