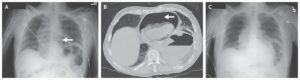
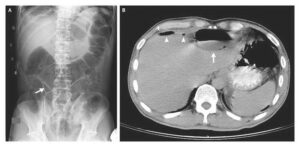
This post is an answer to the Case – 70-year-old Man With Painful, Pruritic Rash
A lesional punch biopsy for routine histology was done and perilesional punch biopsy for direct immunofluorescence. Clinicopathological findings were diagnostic of pemphigus foliaceus.
The patient was prescribed 30 mg prednisolone daily and rituximab (375 mg/m2 intravenously once weekly for 4 weeks), and triamcinolone 0·1% cream twice daily. At follow-up 2 months after treatment with rituximab most skin lesions were healed and prednisolone was reduced to 20 mg daily.
Discussion
Pemphigus foliaceus is a rare autoimmune bullous disease characterised by pathogenic autoantibodies against desmoglein-1 (a desmosomal protein) that cause disruption of intercellular adhesion between keratinocytes in the epidermal granular layer (acantholysis). This results in fragile bullae that rupture easily to form erosions with characteristic scale crust.
Pemphigus foliaceus often begins on the upper body in a seborrheic distribution, but progresses to widespread involvement or erythroderma if not appropriately treated. Pruritus and burning are common and can be exacerbated by UV exposure. Unlike pemphigus vulgaris, pemphigus foliaceus is rarely associated with mucosal involvement.
Diagnosis is made with biopsies for routine histology and direct immunofluorescence. Pemphigus foliaceus typically arises in middle age and can be drug-induced, such as by penicillamine and angiotensin-converting enzyme inhibitors. An endemic form, Fogo Sevelagem (“wild fire”), occurs in South America and has been linked with exposure to black flies.
Before effective treatment was available pemphigus foliaceus fatality reached 60% due to dehydration and sepsis. Rituximab, an anti-CD20 monoclonal antibody, has recently gained favour as treatment of choice for pemphigus foliaceus and other autoimmune bullous diseases because of relatively high rates of induced remission compared with classic treatments.