This post is an answer to the Case – Swollen Legs
What is this condition called, and how is it classified?
She has lymphoedema of the legs. Lymphoedema can be classified into:
- Primary lymphoedema: There is some congenital defect of the lymphatic drainage of the limb.
- Secondary lymphoedema: There is some extrinsic cause producing lymphatic obstruction.
Causes of secondary lymphoedema
- Blockage of the lymphatics and lymph nodes by metastatic tumour deposits, or following radiotherapy to, or block dissection of, involved nodes. This is not uncommonly seen in the arm of patients with advanced breast cancer, for example.
- Secondary to severe bacterial or parasitic infection. Filariasis, caused by Wuchereria bancrofti infestation of the lymphatics, is the cause of gross lymphoedema of the legs, and often the scrotum, in the tropics.
How is primary lymphoedema further subdivided?
- Lymphoedema congenital: As the name suggests, the congenital form. The child presents with swollen legs at about the first year of life. The leg, or legs, may be affected right up to the groin. It is rather more common in males and in about 10% there is a family history. This familial form is known as Milroy’s disease.
- Lymphoedema praecox: This first appears in children or in adults up to the early thirties, with a 3 : 1 predominance in females. The onset peaks at about the menarche, as in our present case, and usually only affects the leg up to the knee, again as occurs here. When a family history is positive, the condition is termed Meig’s disease.
- Lymphoedema tarda: This commences after the age of 35. It is important to exclude the secondary causes of lymphoedema, listed above, in these cases, and also to consider whether the cause may be a previous deep vein thrombosis leading to chronic venous oedema.
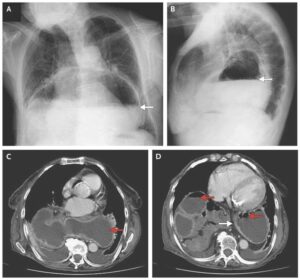
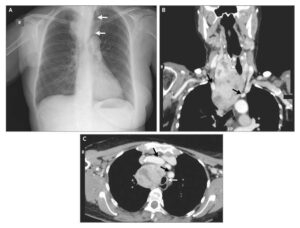
Methylene blue was injected subcutaneously into the dorsum of the patient’s left foot 24 h previously. What do you notice now on the image?
The dye has persisted. This confirms the virtual absence of lymphatic drainage from the foot. In the normal subject the dye would rapidly disappear over a few hours.

What is the aetiology of primary lymphoedema?
Lymphangiographic studies – performed in the 1950s by placing a very fine cannula into a foot lymphatic and visualized by methylene blue injection – defined the congenital anomalies that might affect the lymphatics of the lower limb. These might show aplasia (almost total absence), hypoplasia or varicose dilatation of the lymphatic channels (megalymphatics).
How can this condition be treated?
- The great majority of patients are treated conservatively. This includes elevation of the legs when the subject is sitting down or in bed (heels higher than the knees, knees higher than the hips) and graduated compression stockings. Many respond to this, which may be supplemented with ingenious intermittent pneumatic compression machines in the physiotherapy department.
- The patient is warned to be careful about scratches and abrasions to the legs. The absence of lymphatic drainage renders the limb susceptible to cellulitis, which may damage residual lymphatics. This might well be the aetiology of cases of lymphoedema tarda. Cellulitis of the limb therefore calls for urgent antibiotic treatment.
- Radical surgical excision of the lymphoedematous subcutaneous tissue, down to the deep fascia, is a major procedure and is only indicated in very advanced and disabling cases.