An 86-year-old man was hospitalized for repeated episodes of septic shock due to methicillin-resistant Staphylococcus aureus (MRSA) pneumonia; he ultimately died of pseudomonal sepsis and pneumonia.
In 1948, the patient had pulmonary tuberculosis and underwent extrapleural pneumonolysis (plombage) with polymethyl methacrylate (acrylic or Lucite) balls. The symptoms of pulmonary tuberculosis resolved after plombage, and the patient had no other serious infections until he was hospitalized for pneumonia 57 years later.
Autopsy revealed that the balls used in plombage (3 to 4 cm in diameter) had become imbedded in fibrous tissue, with pleural calcification and moderate inflammatory changes that were consistent with pneumonia and a history of successfully treated tuberculosis; there was no evidence of active tuberculosis.
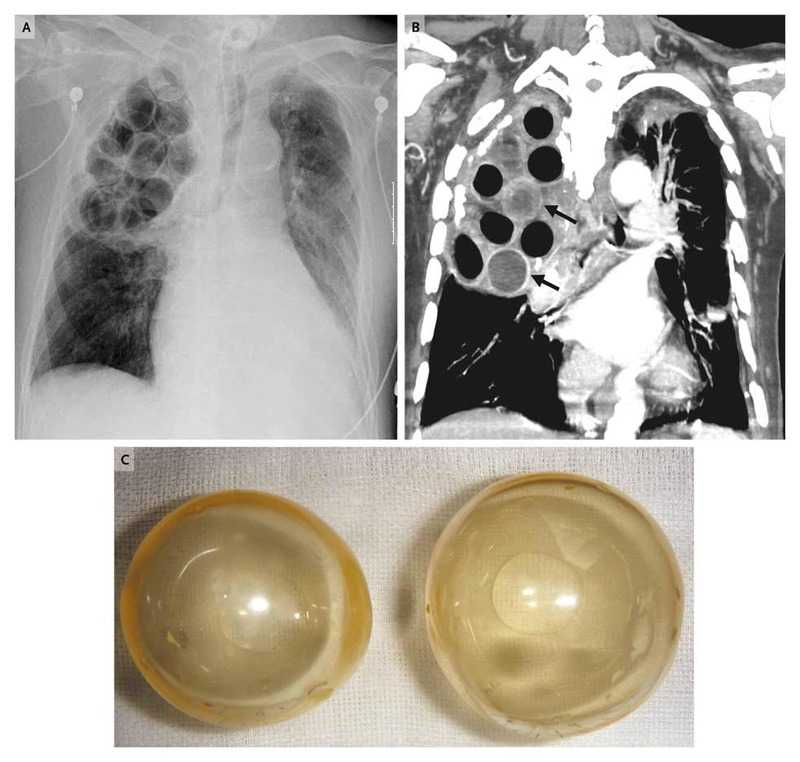
Radiographic and computed tomographic (CT) images of the chest (Panels A and B, respectively) revealed the balls, most of which were lucent (Panel C) and some of which had broken inside the pleural space.
Muddy fluid was observed inside some of the balls, which was consistent with the high-density fluid seen inside the balls on the CT image (arrows in Panel B). Pseudomonas aeruginosa was cultured from both the fluid in the balls and the patient’s blood.
Late complications associated with the plombage procedure include:
- Hemorrhage
- Infection
- Fistula formation