A 47-year-old homeless man presented to the emergency department 1 week after the onset of chest pain. He was hemodynamically stable. The physical examination was unremarkable.
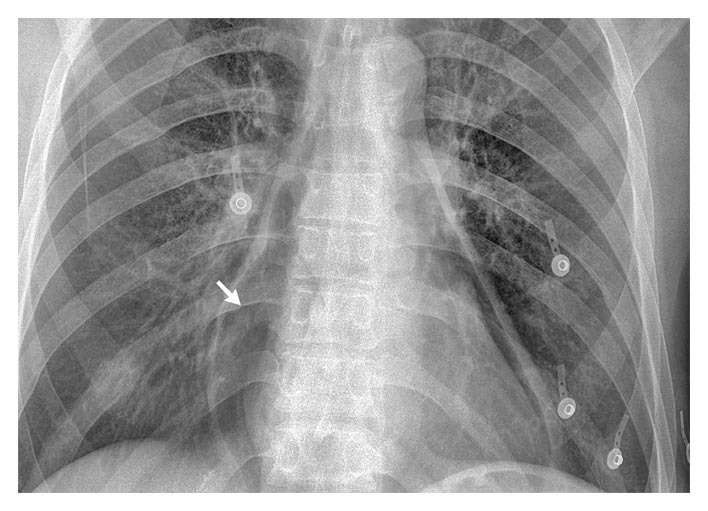
A routine complete blood count revealed 27,000 leukocytes per cubic millimeter. A chest radiograph showed pneumopericardium (arrow) without evidence of pneumothorax or pneumomediastinum.
A computed tomographic scan of the chest confirmed the diagnosis of pneumopericardium and showed circumferential wall thickening of the distal esophagus with an associated esophagopericardial fistula.
Esophagoscopy revealed a deep esophageal ulcer 4.5 cm in diameter, 36 cm from the incisors; the pericardial cavity and the lining of the columnar epithelium could be directly visualized to the distal 10 cm of the esophagus.
Esophageal-biopsy specimens showed intestinal metaplasia with inflammation and high-grade dysplasia. The diagnosis was Barrett’s esophagus.
The patient was taken to the operating room, where lavage and drainage of the pericardium were performed, a pericardial patch and an esophageal stent were placed, and jejunostomy was performed. The patient’s postoperative course was uneventful, and 11 months later, the patient was well.