Definition, Diagnosis, and Clinical Features
Magnesium is the only ion discussed in this chapter that does not have its own hormonal system for regulation. Although PTH has some influence on magnesium excretion and magnesium also on PTH secretion, there is no strict negative feedback loop.
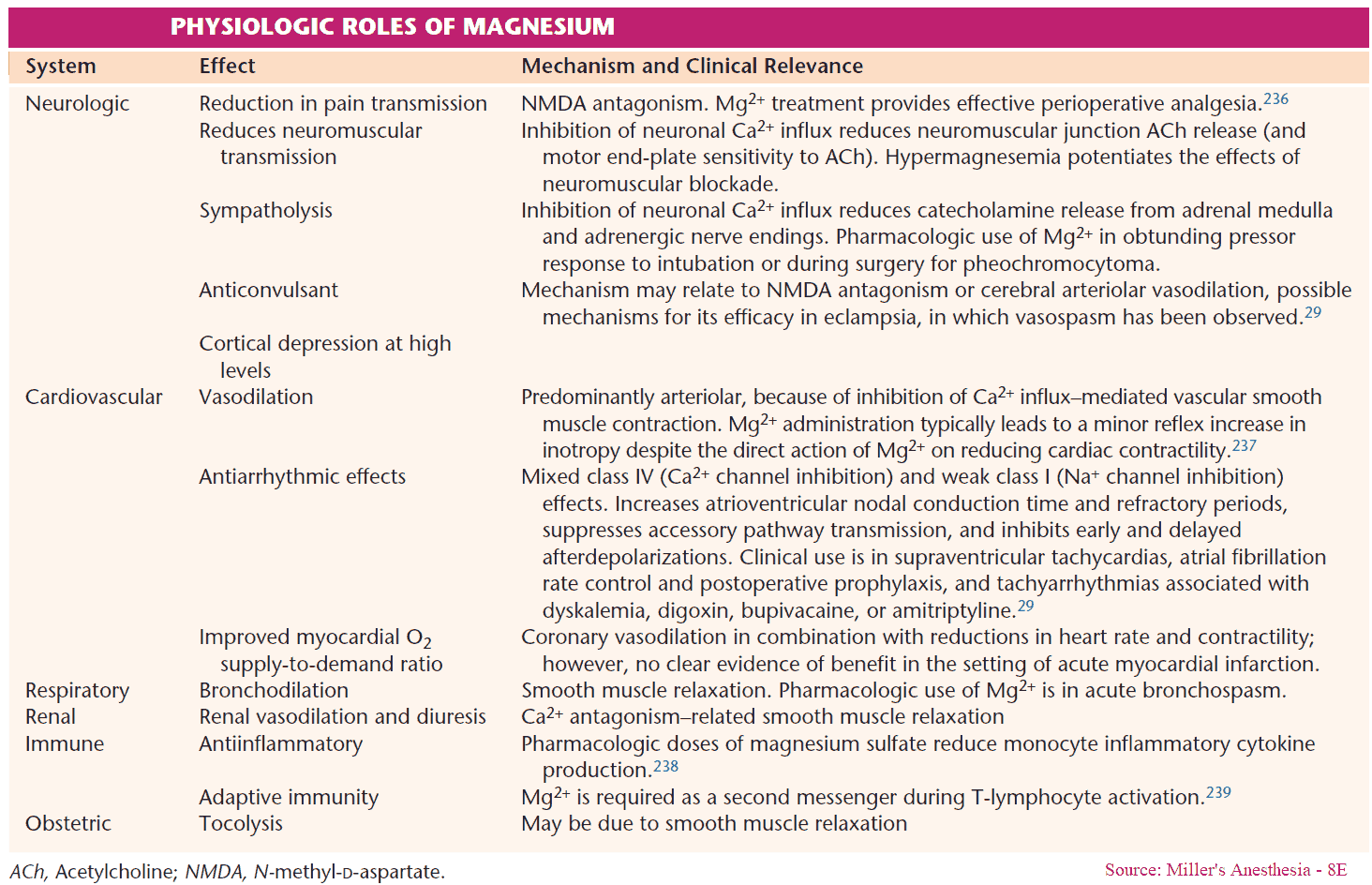
This is rather astonishing since magnesium plays an important role in membrane excitability and also in several intracellular functions (e. g., cofactor for many enzymes involved in protein and nucleic acid synthesis). Renal magnesium excretion is stimulated by hypercalcemia, hypophosphatemia, and hypermagnesemia itself.
Hypomagnesemia is defined as a decrease of serum magnesium levels to 0.8 mmol/L, and hypermagnesemia, as an increase to 1.2 mmol/L.
Diagnosis
Similarly to calcium, a fraction of magnesium in serum is protein-bound (about 30%) and a fraction is complexed (about 15%). Alternative measurement techniques have been evaluated, e. g., measurement of intracellular magnesium levels in erythrocytes and measurement of ionized magnesium in serum, without clear advantages of either method being found. Therefore, the measurement of total magnesium in serum has remained the standard test.
Similarly to calcium, a formula for correction of magnesium levels in patients with hypoalbuminemia has been suggested: ΔMg (mmol/L) = 0.005 × Δalbumin (g/L).
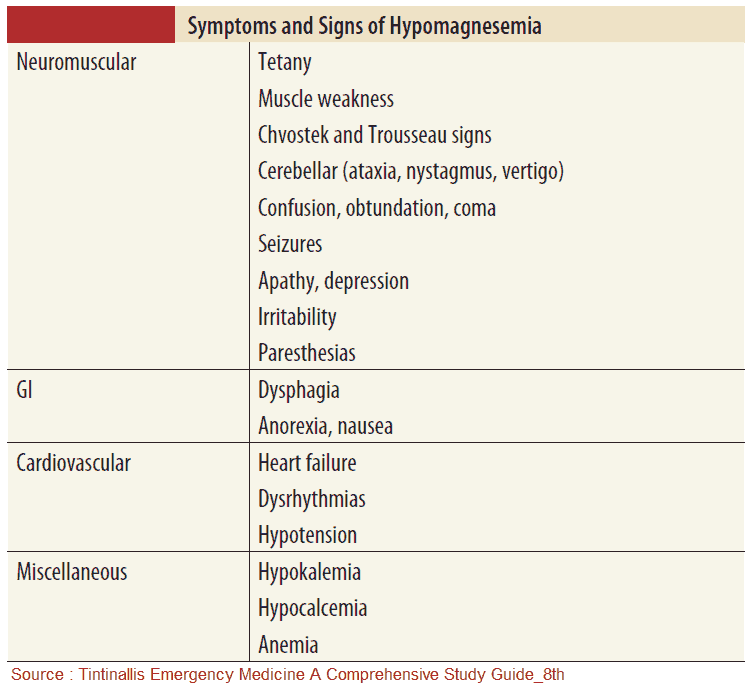
Clinical Features
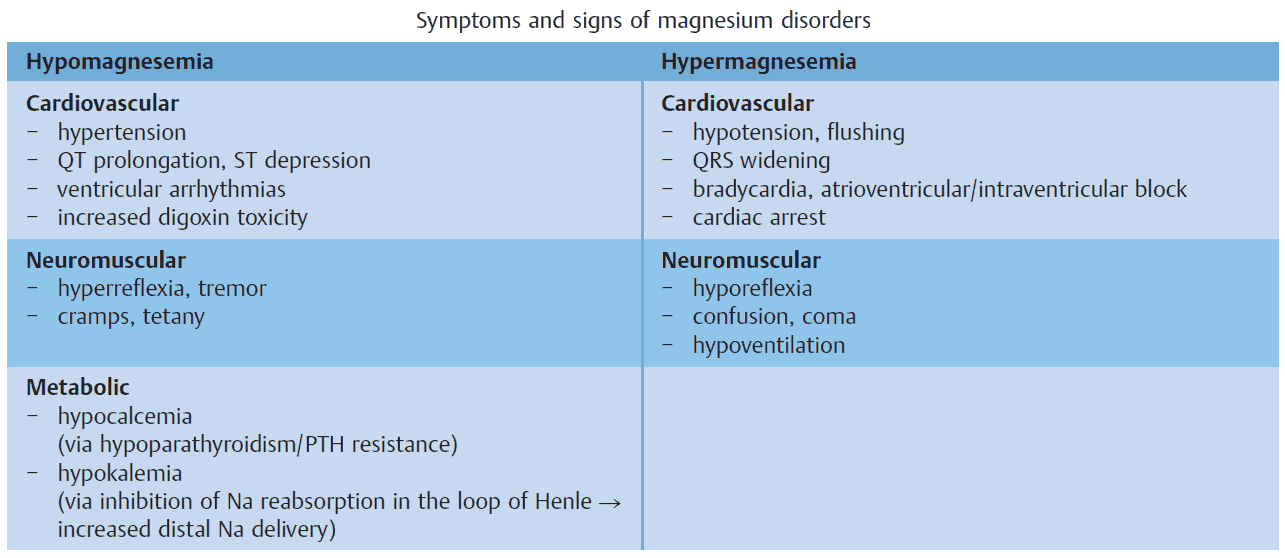
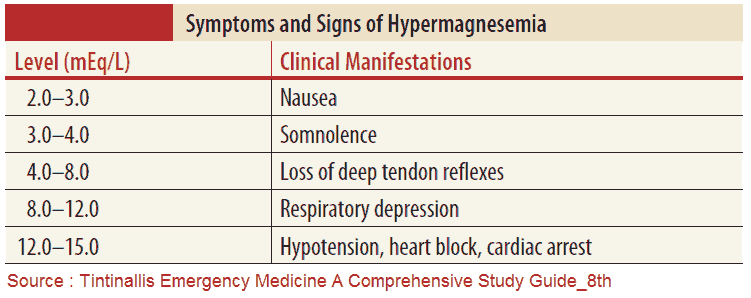
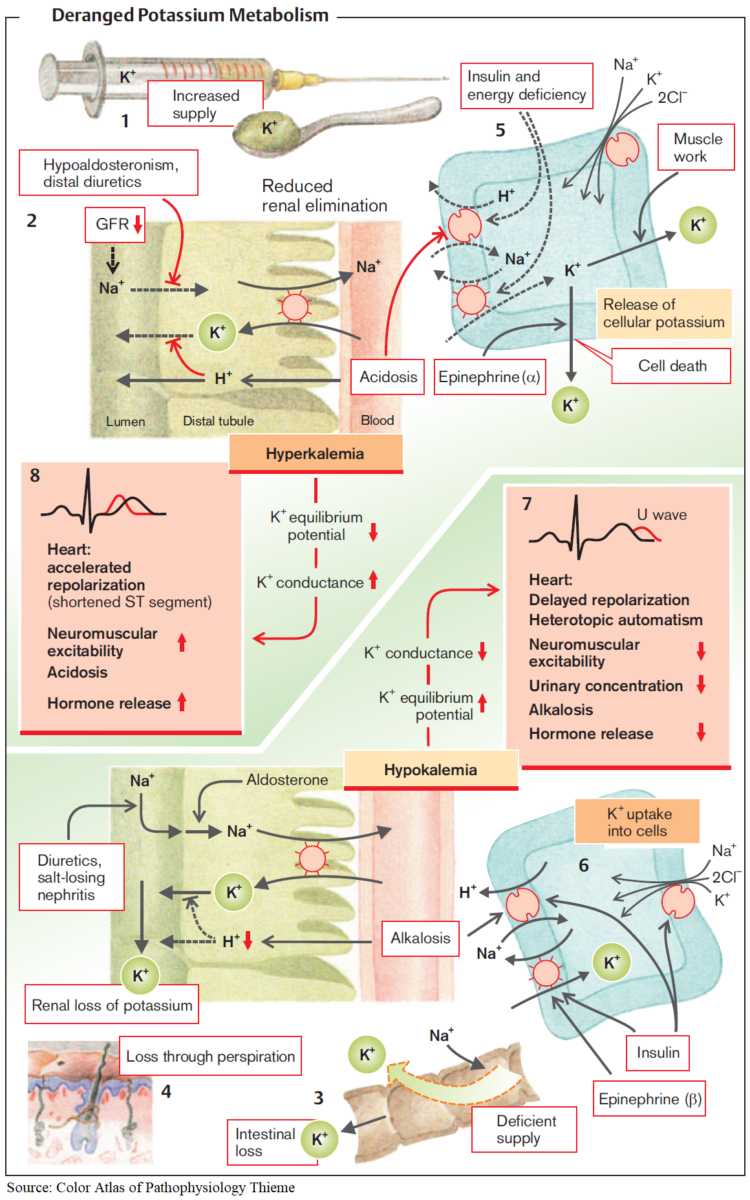
The hallmarks of magnesium disorders are symptoms and signs of altered membrane excitability in heart and skeletal muscles and in the nervous system. They are summarized in the image below.
Magnesium disorders are often associated with other electrolyte disorders (e. g., potassium and calcium). Since these disorders also influence membrane excitability, the symptoms and signs can often not be clearly separated.
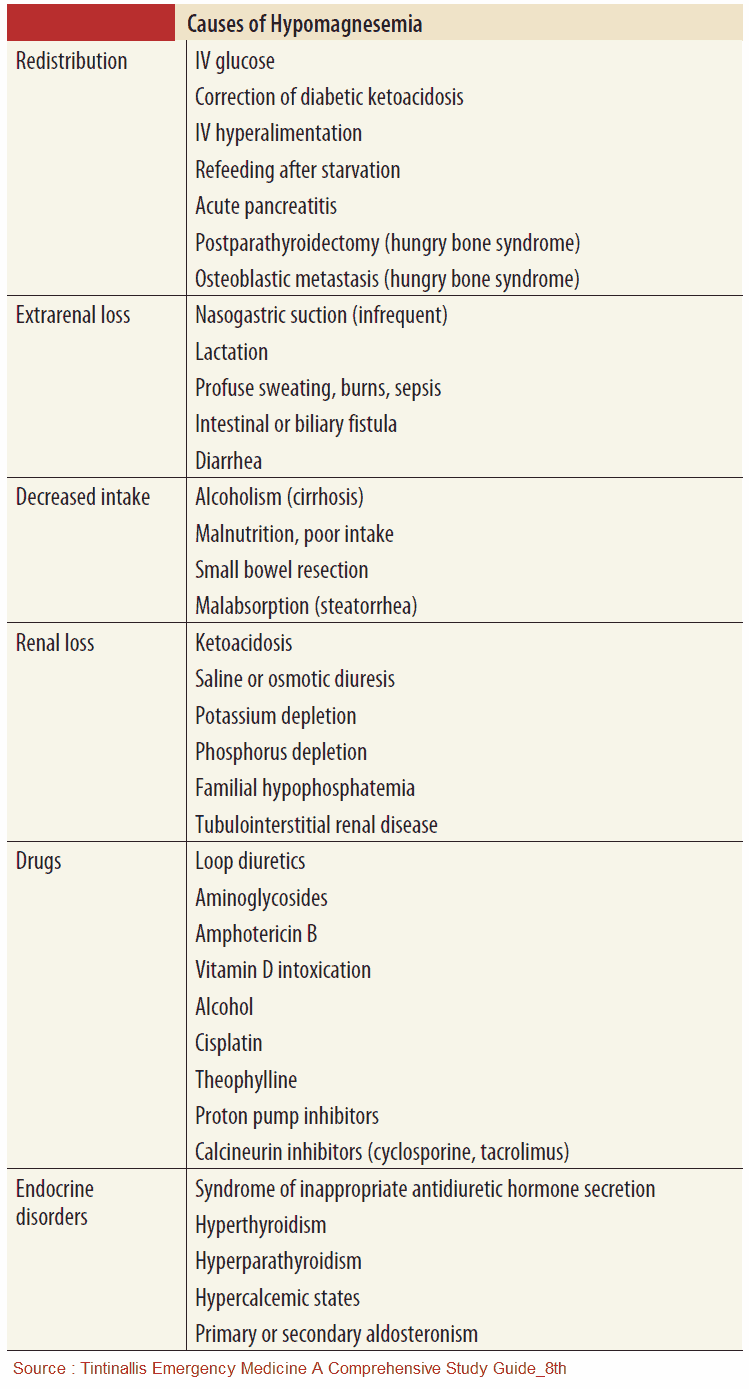
Causes
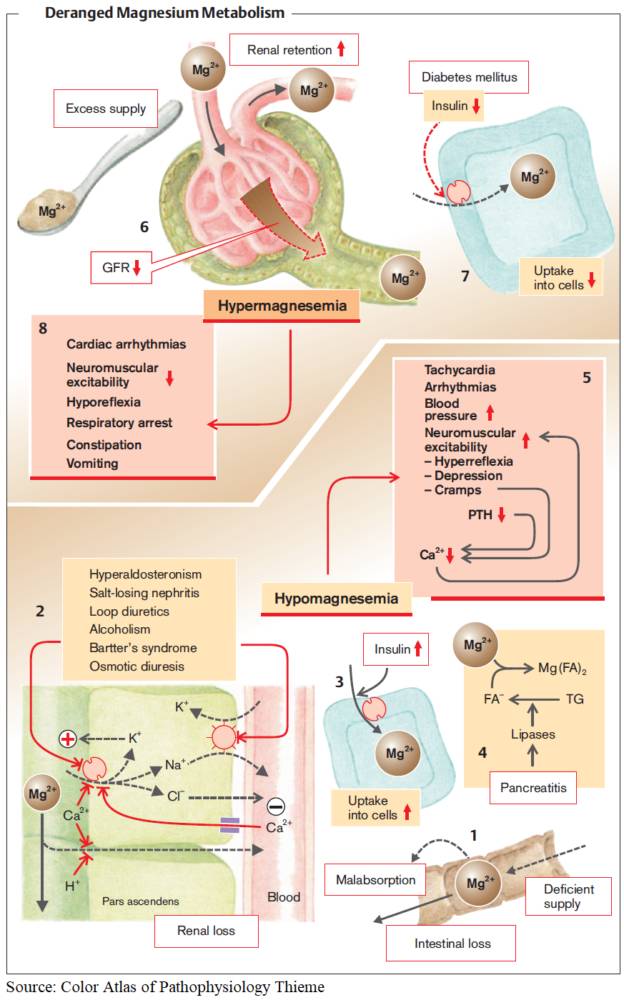
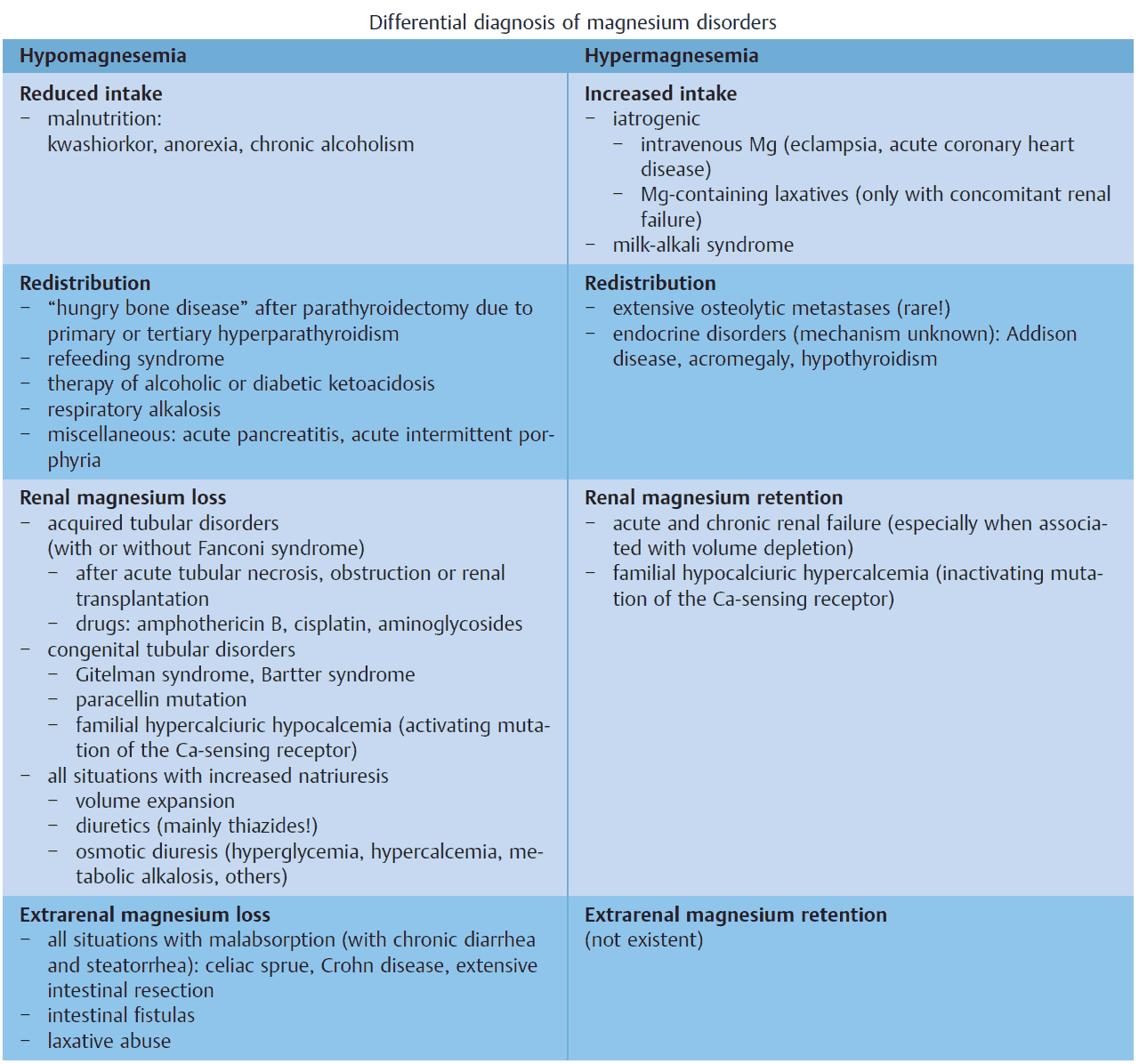
Magnesium disorders can be classified according to pathophysiology:
- disorders of magnesium intake
- transcellular magnesium shifts
- disorders of renal and extrarenal magnesium excretion.
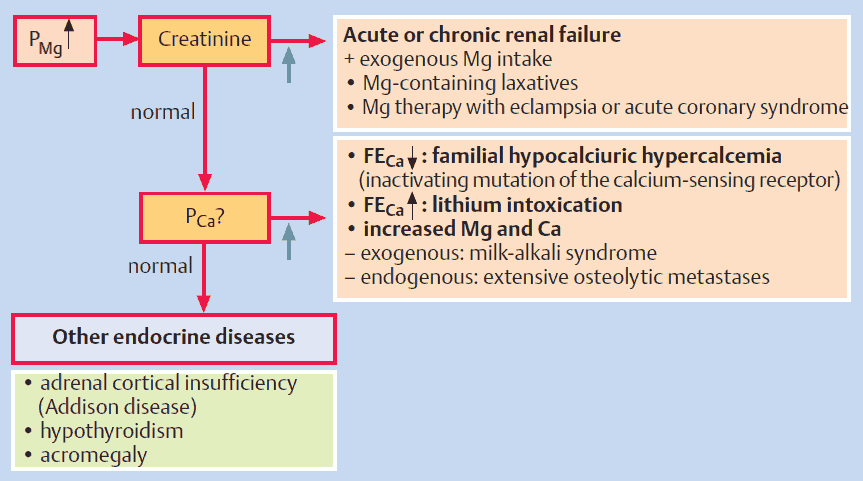
The differential diagnosis of each group is listed in the image below.
Hypomagnesemia (PMg < 0.7 mmol/L)
Causes of Hypomagnesemia
Reduced Intake
This situation is observed with all forms of malnutrition e. g., kwashiorkor, anorexia, and chronic alcoholism. In addition, diseases associated with malabsorption (e. g., celiac sprue, Crohn disease) may lead to hypomagnesemia. Especially in patients with steatorrhea, the divalent calcium and magnesium ions are bound by nonabsorbable fatty acids and are therefore lost in the intestine.
Transcellular Magnesium Shifts
Shifts from the extracellular to the intracellular space occur, analogous to potassium and PO4 3–, in the following situations:
- refeeding syndrome
- herapy of diabetic and alcoholic ketoacidosis
- acute respiratory alkalosis (hyperventilation).
Shifts from the extracellular space to the bones or to soft tissues occur, analogous to calcium, in the following situations:
- “hungry bone disease” (after parathyroidectomy or with vitamin D therapy of severe rickets)
- acute pancreatitis.
Extrarenal Magnesium Loss
Intestinal magnesium loss is observed with chronic diarrhea, laxative abuse, or fistulas.
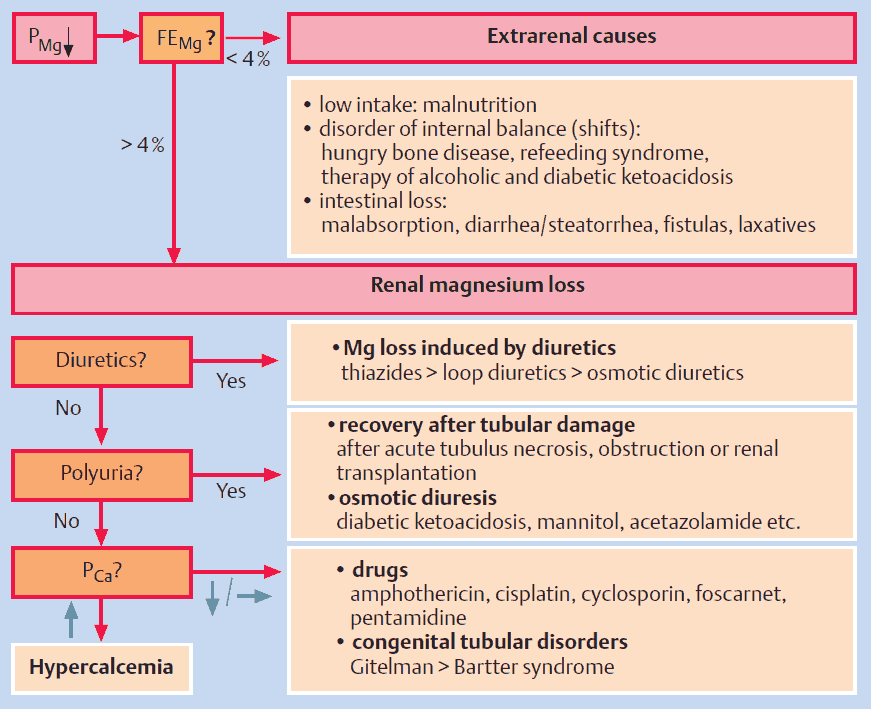
Renal Magnesium Loss
Renal magnesium loss is found in the following situations:
- proximal tubular damage (with or without Fanconi syndrome), e. g., after acute tubular necrosis
- congenital tubular disorders: Gitelman syndrome (magnesium loss = important feature), Bartter syndrome (magnesium loss = less important), paracellin defect
- all situations with increased natriuresis, since magnesium reabsorption is linked with sodium reabsorption, e. g., osmotic diuresis (glucosuria), hypercalciuria, bicarbonaturia, therapy with diuretics.
Symptoms and Signs of Hypomagnesemia
Treatment of Hypomagnesemia
Mild / asymptomatic:
- Oral magnesium salts (e.g., magnesium oxide, magnesium gluconate)
- Divide doses to reduce diarrhea risk
Moderate to severe or symptomatic (tetany, arrhythmias, seizures):
- IV magnesium sulfate
- Typical: 1–2 g over 15–60 min for acute symptoms
- Continuous infusion may be needed for sustained correction
Concomitant electrolyte disturbances:
- Correct hypokalemia and hypocalcemia (often resistant until Mg²⁺ is repleted)
Underlying cause:
- Address GI losses, renal wasting (e.g., diuretics, cisplatin), alcoholism, malnutrition
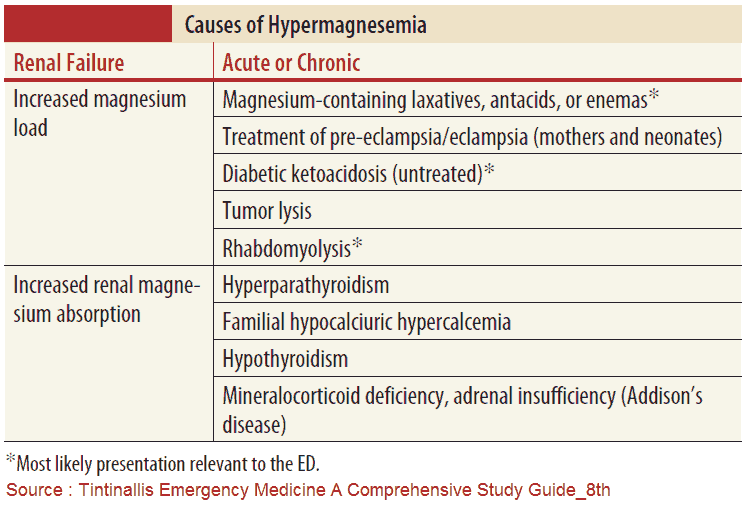
Hypermagnesemia (PMg > 1.2 mmol/L)
Causes of Hypermagnesemia
Increased Intake
Hypermagnesemia is rare and occurs almost exclusively with exogenous intake. High-dose magnesium is given for therapy of eclampsia. Other exogenous sources are magnesium-containing laxatives and milk, in the context of milk-alkali syndrome. However, similar to PO4 3– and potassium, renal magnesium excretion is very efficient, and therefore hypermagnesemia only occurs if renal function is impaired and/or volume depletion is present.
Transcellular Magnesium Shifts
Hypermagnesemia rarely occurs with diffuse and extensive osteolytic metastases and also in the context of various endocrine diseases, especially with adrenal insufficiency. The pathogenesis in the latter situation is unclear.
Renal Magnesium Retention
Acute and chronic renal insufficiency with concomitant magnesium intake can lead to hypermagnesemia. A rare genetic cause for hypermagnesemia is the familial hypocalciuric hypercalcemia with an inactivating mutation of the calcium-sensing receptor.
Symptoms and Signs of Hypermagnesemia
Treatment of Hypermagnesemia
Mild / asymptomatic (Mg²⁺ < 4 mmol/L):
- Stop magnesium-containing drugs (antacids, laxatives, supplements)
- IV hydration with isotonic saline
- Loop diuretics to enhance Mg²⁺ excretion (if renal function intact)
Moderate to severe / symptomatic (loss of reflexes, hypotension, arrhythmias, respiratory depression):
- Cardiac/neuromuscular stabilization: IV calcium gluconate (antagonizes magnesium’s effects)
- Enhance elimination:
- Loop diuretics + IV fluids (if renal function preserved)
- Hemodialysis in renal failure or refractory cases
Supportive care:
- Mechanical ventilation if respiratory compromise
- Vasopressors if severe hypotension
References
- Cole DE et al. Inherited disorders of renal magnesium handling. J Am Soc Nephrol 2000; 11:1937–47.
- Crook MA et al. The importance of the refeeding syndrome. Nutrition 2001; 17:632–63.
- Konrad M et al. Insights into the molecular nature of magnesium homeostasis. Am J Physiol Renal Physiol 2004; 286:F599–605.
- Weisinger JR, Bellorin-Font E. Electrolyte quintet: magnesium and phosphorus. Lancet 1998; 352:391–6.