Table of Contents
When a patient with undifferentiated shock presents to the emergency department, physicians are forced to make rapid management decisions based on limited information about the patient’s history or recent course of illness.
Ultrasound has emerged as an effective diagnostic tool that bedside physicians can use to get actionable information on the etiology of hypotension, as well as actively guide resuscitation and monitor potential improvement in the patient’s clinical status.
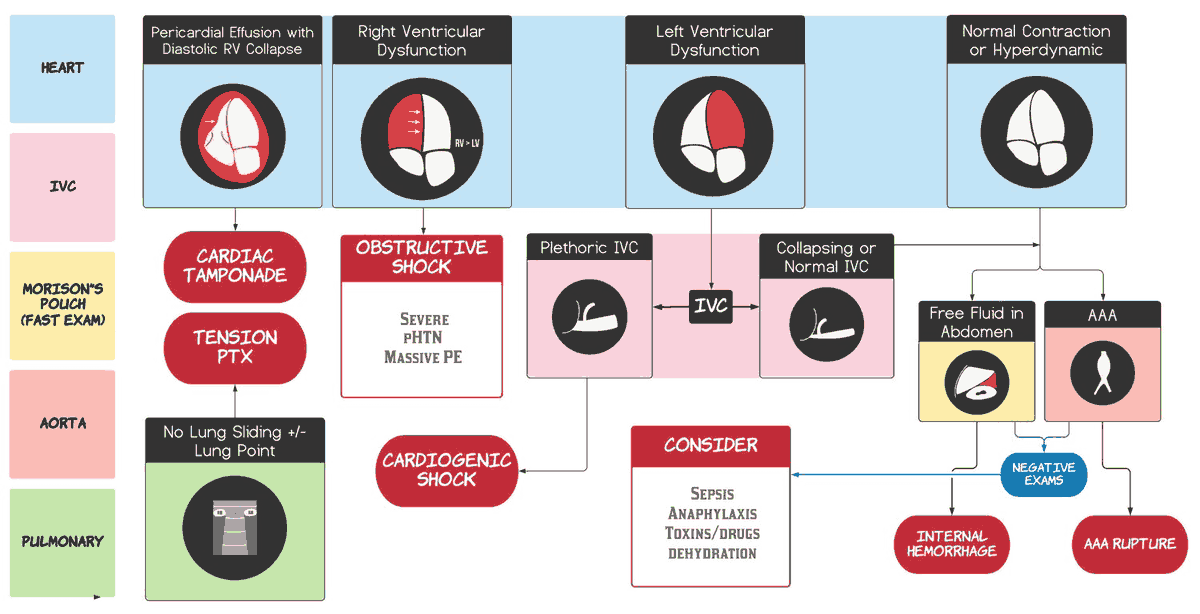
While many ultrasound protocols have been developed to aid in resuscitating critically ill patients, the Rapid Ultrasound in Shock or RUSH exam has risen in prominence due to its ability to rapidly and accurately diagnose the classification of shock. This exam takes a three-step bedside protocol to assess a critically ill patient’s cardiovascular status (“the pump”), intravascular volume status (“the tank”), and vascular integrity (“the pipes”).
This protocol integrates several familiar ultrasound applications that the emergency physician can perform in real time at the bedside to guide resuscitative efforts for patients in shock. The three steps of the RUSH exam are explained in further detail below.
“The Pump” – Assess the Cardiovascular Status
The first step in performing the RUSH exam on a patient in shock is a cardiac examination of “the pump.” The physician assesses the heart for pericardial effusion in the most dependent portion of the pericardium with a subxiphoid view. A large pericardial effusion may suggest cardiac tamponade, which in an unstable hypotensive patient indicates the need for emergent pericardiocentesis to relieve obstructive shock.
This investigation then proceeds to parasternal long and parasternal short axis views of the heart to assess cardiac contractility. A gross visual inspection of cardiac dynamics and wall excursion can be used to classify cardiac contractility as normal, reduced, hyperdynamic, or absent. A hyperdynamic heart with good contractility suggests hypovolemic or distributive shock that may benefit from a fluid bolus, while a hypodynamic heart with reduced contractility indicates cardiogenic shock that may benefit from vasopressors and inotropes.
The final step in assessing “the pump” is to perform an apical four-chamber view, paying special attention to the size of the right ventricular. The right ventricle is normally smaller than the left ventricle. An acutely enlarged right ventricle should raise suspicion for obstructive shock caused by a massive pulmonary embolism.
“The Tank” – Assess Intravascular Volume Status
The second step in performing the RUSH exam is to evaluate the patient’s intravascular volume status, that is, “the tank,” for fullness, leakiness, compromise, or overload, which is described below.
“Tank Fullness” – Evaluation of the Inferior Vena Cava for Size and Collapsibility
Using a phased-array or curvilinear probe, the fullness of the tank can be evaluated by measuring the inferior vena cava (IVC) width and assessing for collapsibility with inspiration. An IVC width < 2 cm and collapsibility > 50% of the vessel diameter during inspiration suggest decreased intravascular volume.
In the setting of hypotension, these findings can indicate distributive or hypovolemic shock. After administering a fluid bolus, this exam may be repeated to determine any improvement in IVC diameter or collapsibility.
Alternatively, an IVC width > 2 cm in combination with decreased cardiac contractility may suggest cardiogenic shock. As a caveat, measuring IVC in an intubated patient becomes unreliable due to increased intrathoracic pressure.
“Tank Leakiness” – Evaluation with Extended FAST Exam
The next sequence is evaluating “the tank” for leakiness by performing an Extended Focused Assessment with Sonography in Trauma (eFAST) exam to assess the abdomen for intraperitoneal free fluid and the bilateral lung bases for thoracic fluid, which could represent hemothorax in the appropriate clinical setting. Consideration should be given to conditions such as traumatic injuries, ruptured ectopic pregnancy, ruptured ovarian cyst, or ruptured abdominal aortic aneurysm that cause hemorrhagic shock.
“Tank Compromise” – Evaluation for Pneumothorax
After completing the abdominal portion of the eFAST exam, evaluation of the “the tank” progresses to an assessment of the lungs with a linear probe. The presence of bilateral lung sliding and comet tail artifact rules out hypotension due to tension pneumothorax causing obstructive shock.
“Tank Overload” – Evaluation for Pulmonary Edema
The phased-array or curvilinear probe may then be used to assess the thorax for B-lines, which if present bilaterally are suggestive of pulmonary edema due to cardiogenic shock.
“The pipes” – Assess Vascular Integrity
The final step of the RUSH exam on a hypotensive patient is to evaluate the vascular system or “the pipes.” Using a low-frequency probe, the proximal, middle, and distal abdominal aorta should be examined for a diameter >3 cm, which is indicative of an aneurysm. The presence of an aortic aneurysm may suggest a ruptured aortic aneurysm as the etiology of hypotension.
The lower extremity veins can also be assessed using a linear probe for the presence of deep vein thrombosis. This study should investigate the common femoral vein down through its bifurcation and the popliteal vein in the popliteal fossa for the presence of a thrombus. Deep vein thrombosis in the lower extremities may represent massive pulmonary embolism and obstructive shock as a possible etiology of hypotension. The diagnosis may be supported by the presence of an enlarged right ventricular and right heart strain visualized on the ultrasound.
The undifferentiated hypotensive patient can present a challenge for the emergency physician, requiring decisive action with limited information during resuscitation. A RUSH exam can provide a quick and noninvasive evaluation of “the pump,” “the tank,” and “the pipes” to help determine the etiology of hypotension. Be inspired to perform bedside ultrasound for your next hypotensive patient to rapidly and easily gain valuable clinical information and help guide management of the resuscitation.
Key Points
- RUSH to resuscitation in the undifferentiated hypotensive patient.
- Evaluate “the pump” for pericardial effusion, contractility, and signs of right ventricular strain.
- Evaluate “the tank” for IVC size and collapsibility, intraperitoneal free fluid, pleural fluid, pneumothorax, and pulmonary edema.
- Evaluate “the pipes” for aortic aneurysm and deep vein thrombosis.
- Reevaluate after interventions to assess changes in volume status and cardiac contractility.