Anaphylaxis is a serious systemic IgE-dependent immunologic hypersensitivity reaction, potentially fatal without early detection and management. Anaphylaxis tends to be underrecognized and undertreated with a lifetime prevalence based on international studies estimated to be at 0.05% to 2%.
Based on the World Allergy Organization guidelines published in 2011, anaphylaxis is diagnosed if any of the following three criteria are met:
- Onset of illness involving skin or mucosal tissue with respiratory compromise or reduced blood pressure
- An exposure to a likely allergen with the development of two of the following: skin or mucosal tissue involvement, reduced blood pressure, respiratory compromise, or persistent gastrointestinal (GI) symptoms
- Reduced blood pressure after exposure to a known allergen
Main allergy triggers differ by age group and geographical region. Food is the most common precipitant of anaphylaxis in pediatric and young adult populations, while insect stings and medications are more common precipitants in middle-aged and elderly adults. Be sure to ask about all exposures and events in the hours preceding the onset of symptoms. Remember that different patient factors contribute to the severity of anaphylaxis, namely, age, comorbidities, and concurrent medications.
Epinephrine is First-Line Treatment for Anaphylaxis
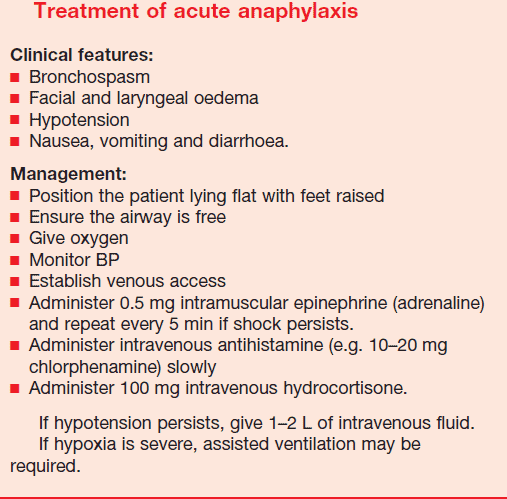
As with any patient, the approach to treatment must be systematic. Start by removing any exposure to the trigger if it is still present, while rapidly addressing the patient’s airway, breathing, and circulation. If anaphylaxis is suspected, immediate treatment with intramuscular (IM) epinephrine is indicated.
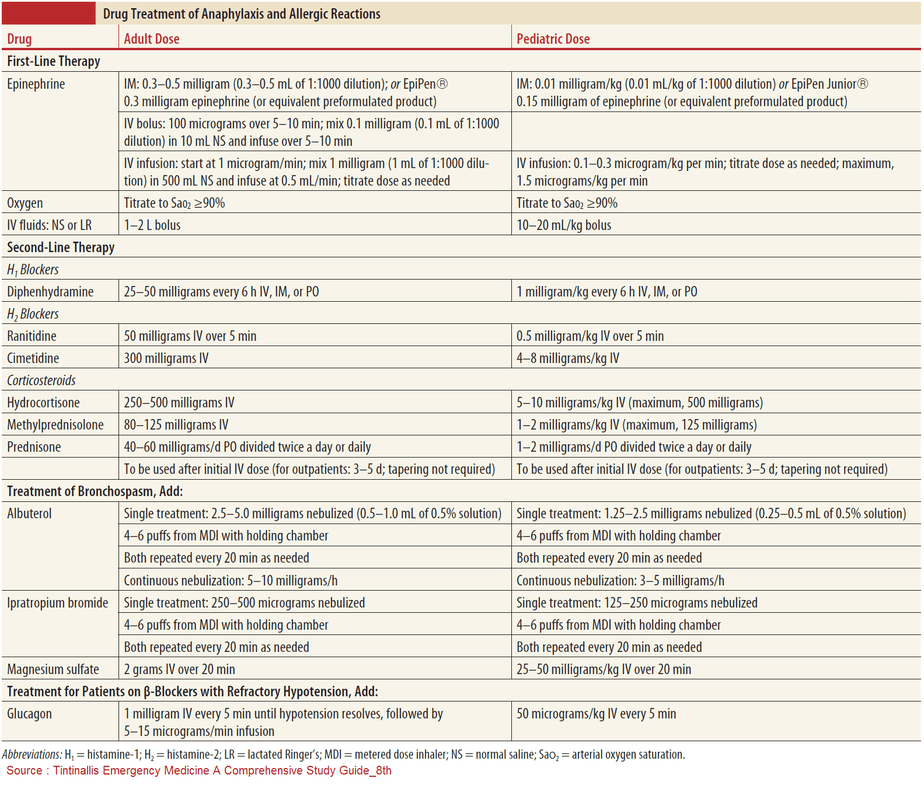
Dosage of Epinephrine in Anaphylaxis
In the setting of anaphylaxis, the pediatric dose of epinephrine is 0.01 mg/kg of a 1:1,000 (1 mg/mL) solution. The adult dose is generally 0.3 to 0.5 mg of 1:1,000 epinephrine solution (0.5 mg is the maximum dose). Note that 0.3 mg is the dose contained in a standard adult epinephrine autoinjector. Depending on the severity of symptoms and the patient’s response to the initial dose, epinephrine can be repeated every 5 to 15 minutes, as needed.
In patients who do not respond to IM epinephrine, assess the intravascular fluid status carefully before progressing to intravenous epinephrine. However, if circulatory shock has developed and cardiac arrest is imminent, administer epinephrine intravenously or intraosseous by slow infusion (1 to 10 μg/min for adults, and 0.1 μg/kg/min for children), titrating it according to hemodynamic parameters.
Complications from IM epinephrine are rare; patients who are elderly or have known cardiovascular disease may also benefit from receiving epinephrine. The benefits from reversing cardiovascular collapse outweigh the risks of hypertension and increased cardiac demand.
Why Does Epinephrine Work ?
Evidence favors prompt epinephrine injection over the use of antihistamines and glucocorticoids for the treatment of anaphylaxis. The therapeutic effect of epinephrine stems from its mechanism of action, as it directly reverses the pathophysiology behind anaphylaxis.
Namely, epinephrine has alpha-1 adrenergic agonist effects, increasing peripheral vascular resistance while decreasing mucosal edema. These critical two effects address potentially lethal hypotension and airway compromise. In addition, epinephrine has beta-1 adrenergic agonist effects increasing heart rate and cardiac contractility and beta-2 adrenergic agonist effects leading to bronchodilation and decreased release of inflammatory mediators from mast cells and basophils.
Failure to inject epinephrine promptly is associated with severe cardiopulmonary compromise and biphasic anaphylaxis with recurrence of symptoms in up to 72 hours. Yet, it is crucial to watch for critical side effects of epinephrine. Rarely, epinephrine may lead to ventricular arrhythmias, acute coronary syndrome, pulmonary edema, and intracranial hemorrhage. Bear in mind that serious adverse effects occur most commonly after rapid intravenous bolus injections or incorrect dosing.
Are there any second-line treatments available ?
Evidence for the administration of second-line medications such as antihistamines, beta-2 adrenergic agonists, and glucocorticoids is extrapolated mainly from their use in treating urticaria (treated by antihistamines) and acute asthma (treated by beta-2 adrenergic agonists and glucocorticoids). Do not focus on those medications if they will delay the prompt administration of epinephrine.
Antihistamines (H1 and H2 blockers) are potentially beneficial to relieve the patient’s itching, flushing, and urticaria. The concerns with using H1 blockers include their potential to cause somnolence and their slow onset of action. Little evidence exists for the concurrent use of H2 blockers.
Beta-2 agonists, unlike epinephrine, help to relieve wheezing, coughing, and shortness of breathe by relaxing smooth muscle. However, beta-2 agonists have no effect on the upper airway edema since no smooth muscles are present there.
Systemic glucocorticoids take several hours to work. Their role is to potentially relieve protracted anaphylaxis symptoms and prevent biphasic anaphylaxis, although these effects have not been proven.
Conclusion
Deciding on the disposition of the patient poses another challenge for clinicians. This decision should be based on the severity of the patients’ symptoms and their prompt response to initial interventions. Patients with moderate respiratory or cardiovascular compromise should be monitored for at least 4 to 6 hours, whereas patients with severe or protracted anaphylaxis may require prolonged monitoring and inpatient admission, ranging from acute short-term to intensive care.
Discharged patients must be informed and educated about recurring symptom(s). Patients should be advised to follow up with their primary care physician and an allergist to confirm the trigger since the key to preventing symptoms is to avoid the allergen.
Explanation should include a description of epinephrine as well as instructions for when and how to self-administer this medication, emphasizing the importance of staying equipped with an epinephrine autoinjector. Discharge instructions should include a prescription for an epinephrine autoinjector if appropriate and also consider a refill for this potentially lifesaving medication. Beware that this device may be prohibitively expensive for the patient and may require social work involvement.
Due to its potential for serious morbidity and mortality, it is essential for emergency medicine clinicians to rapidly recognize and treat anaphylaxis. Furthermore, physicians have a duty to educate patients and their families about how to prevent anaphylaxis and to treat symptomatic patients with lifesaving epinephrine when necessary.
Key Points
- Anaphylaxis in patients is common; recognize its effect on potential organs including skin, mucosa, heart, lungs, and the GI tract and treat promptly.
- Immediately address the airway, breathing, and circulation issues, and keep in mind that patients must be monitored for at least 4 to 6 hours.
- The recommended dose of epinephrine is 0.01 mg/kg of 1:1,000 solution intramuscular (IM). An adult dose generally ranges between 0.3 and 0.5 mg IM.
- Do not delay administering epinephrine when also giving antihistamines or glucocorticoids.
- Educate patients about avoiding allergy triggers and how to use epinephrine autoinjectors.