Table of Contents
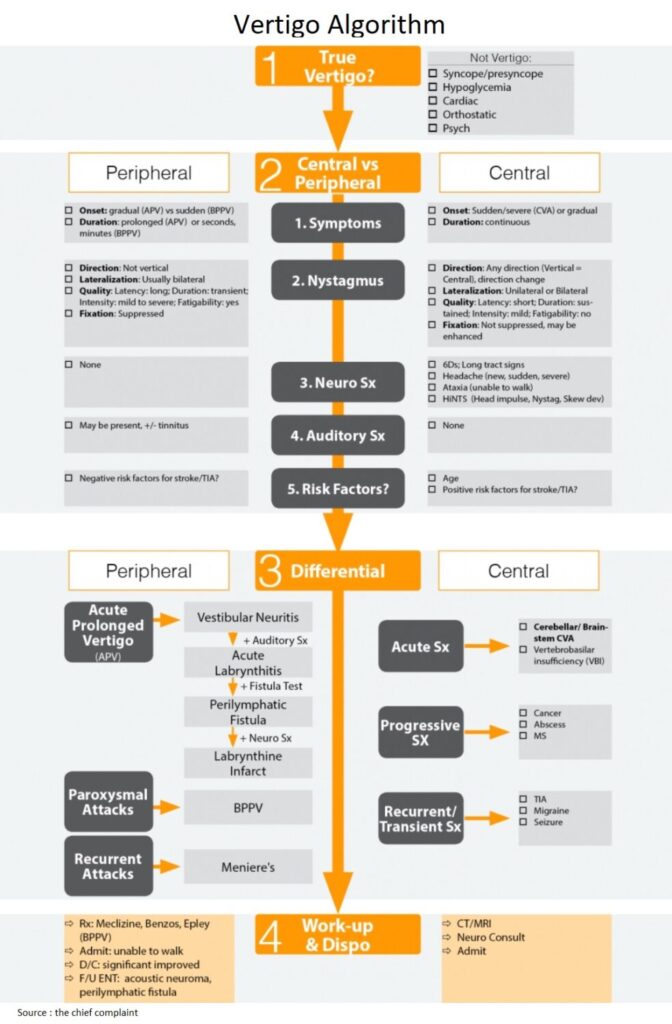
Is it True Vertigo ?
- The Approach (Questions)
- Is the dizziness true vertigo
- If so, is it central or peripheral vertigo
- Is the vertigo intermittent → likely benign
- Constant vertigo is either acute peripheral vestibulopathy (APV) or a posterior circulation/cerebellar CVA
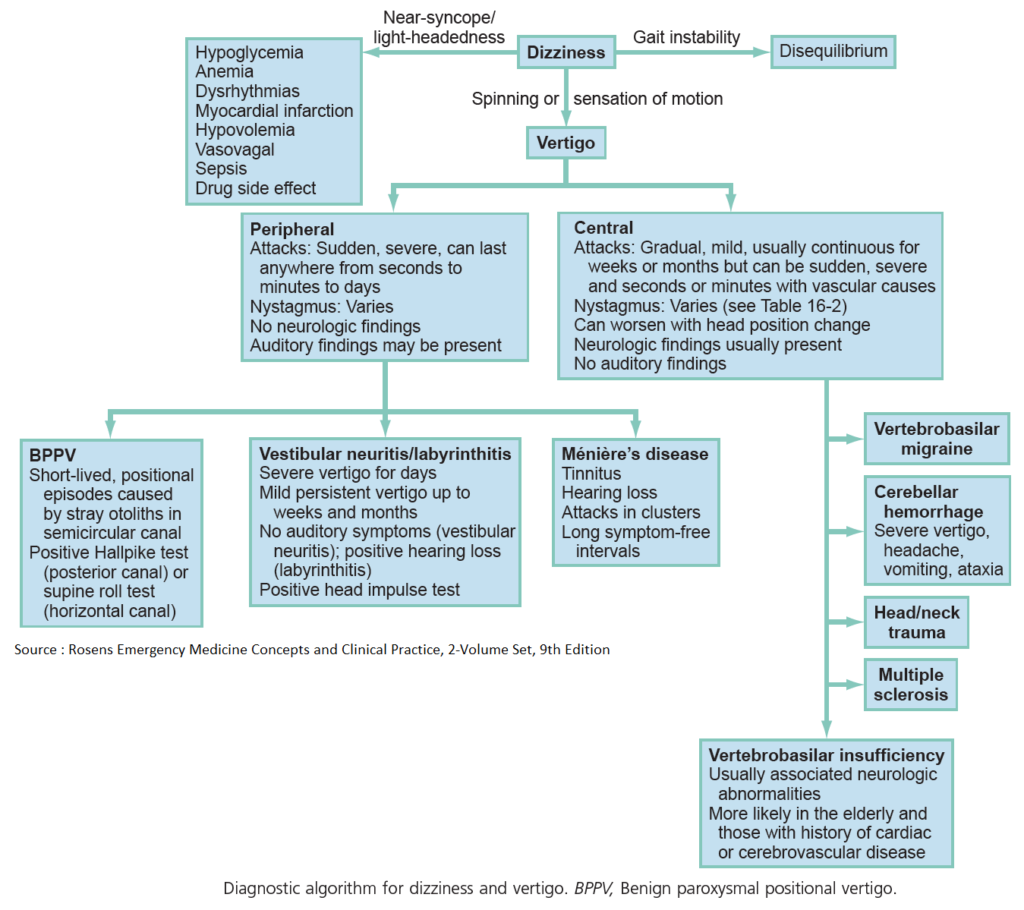
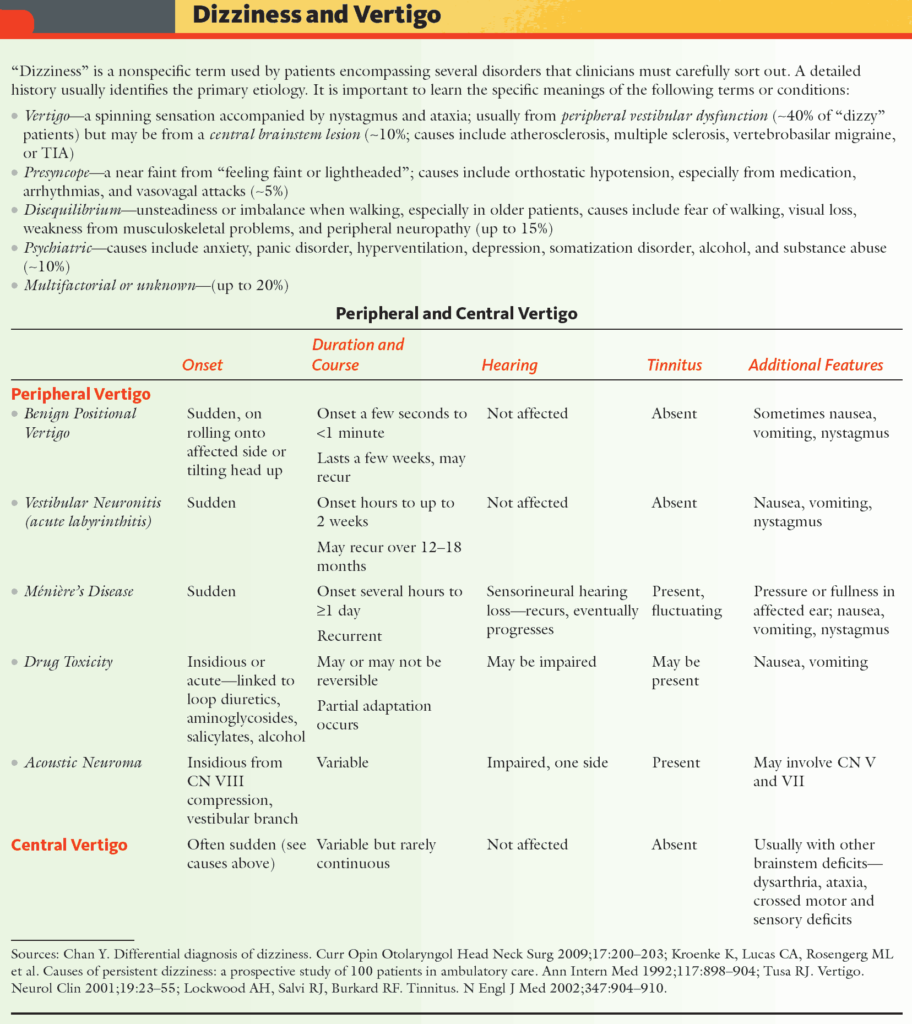
- General Dizziness: 4 different etiologies
- Lightheadedness/Presyncope
- Vertigo
- Dysequilibrium (neuromuscular disorder)
- Psychiatric
- Definitions (Rosen’s Emerg Med, 6th ed. Ch 13. 2006)
- True Vertigo: disorientation in space combined with a sense of motion
- Hallucination of movement of self (subjective vertigo) or of environment (objective vertigo)
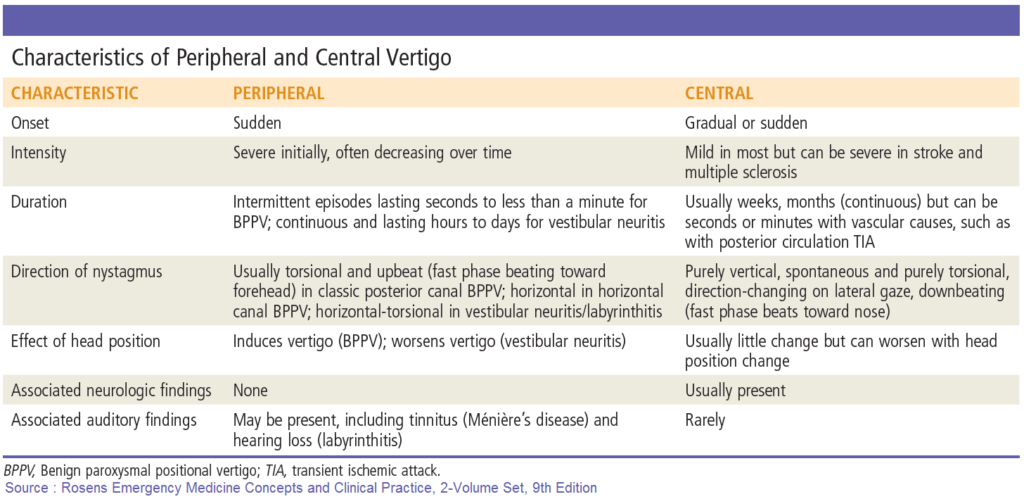
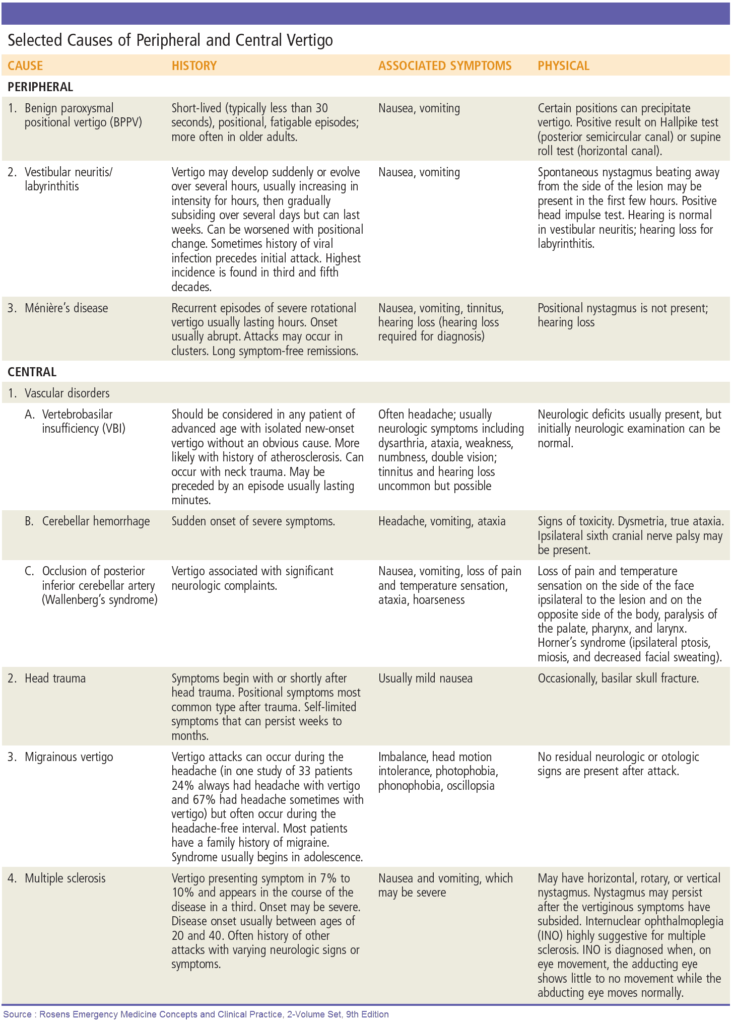
Central vs Peripheral Vertigo
General Approach
- Objective for vertigo is differentiating benign peripheral vertigo from life-threatening central vertigo, using the 5 criteria
Symptoms
- Cerebellar CVA: acute onset and continuous
- Other central vertigo is usually more gradual and continuous
- APV (acute peripheral vestibulopathy): gradual onset and continuous
- BPPV: Acute onset but intermittent
Nystagmus
- Central vertigo:
- Vertical
- Unilateral
- Non-fatigable
- Unsupressed: not suppressed with fixation of gaze (nystagmus persistent when looking straight at your finger)
- Direction change: direction of nystagmus changes with eccentric gaze
- Vertical nystagmus ddx: central vertigo, PCP, EtOH (alcohol), drugs
Neurologic symptoms
- Neuro exam: 6Ds of an abnormal neuro exam:
- Dizziness (vertigo)
- Diplopia (double vision)
- Dysphagia (difficulty swallowing)
- Dysarthria (difficulty speaking)
- Dysmetria (cerebellar ataxia)
- Dysdiadochokinesia (impaired ability to perform rapid, alternating movements)
- Long-tract signs
- Motor/sensory loss
- Ataxia
- Central vertigo/cerebellar pts usually unable to walk
Auditory symptoms
- Auditory symptoms a sign of peripheral vertigo (acute labrynthitis)
6Ds
□ Dizziness
□ Diplopia
□ Dysphagia
□ Dysarthria
□ Dysmetria
□ Dysdiadochokinesia
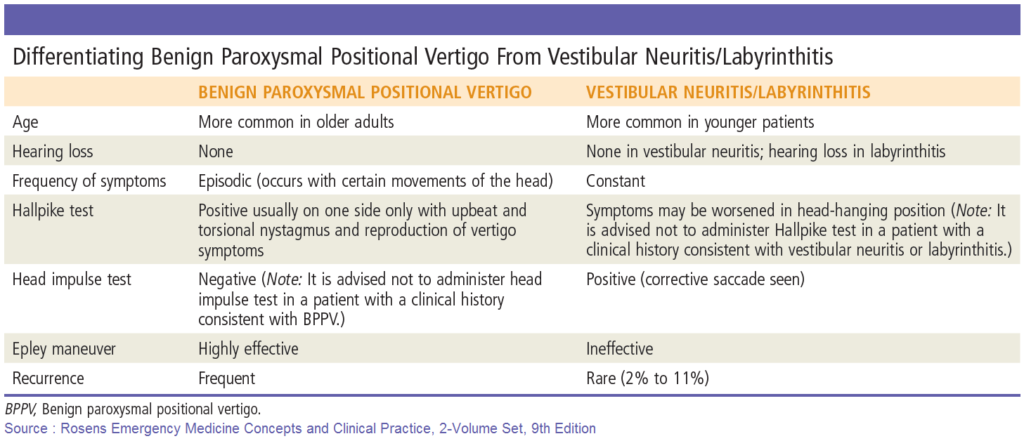
HiNTS Test (Stroke 2009;40:3504-10)
- Head impulse test (Hi): (NEJM 2003;348:1027-32)
- Bedside test of horizontal VOR (vestibuloocular reflex)
- Start: Head turned to one side and eyes turned 10º from center to same side
- Motion: Apply brief high acceleration head turn so that eyes end looking at examiner’s nose
- Test: Catch up saccades on one side, but not the other indicates peripheral vestibular lesion on that side
- Nystagmus (N)
- Nystagmus changes direction on eccentric gaze → central lesion
- Skew deviation (TS)
- Eyes are vertically misaligned because of imbalance of vestibular tone → central lesion
- Alternately cover each eye to test for realignment
- Positive test (central lesion-stroke)
- Normal horizontal head impulse test, direction-changing nystagmus in eccentric gaze, or skew deviation (vertical ocular misalignment)
- HINTS Test 100% sensitive, 96% specific for identifying stroke (Stroke 2009;40:3504-10)
Risk factor Assessment
- Isolated vertigo can be the only symptom in cerebellar stroke/TIA and posterior circulation hemorrhage
- Risk factors: Older age, male sex, and the presence of hypertension, coronary artery disease, diabetes mellitus, and atrial fibrillation
Peripheral vertigo
1. Vestibulopathy (APV)
Definition
- APV= Acute Peripheral Vestibulopathy or Acute Prolonged Vertigo
- Prolonged vertigo definition: continuous vertigo lasting more than a few hours
- Self limited, likely viral cause for symptoms → affecting peripheral vestibular portion of CN8 (Vestibulocochlear nerve)
- Clinical
- Symptoms: gradual onset and continuous vertigo
- Neuro: Normal neuro exam and non-concerning type of nystagmus
- Head thrust test: positive, catch up saccades on one side
VESTIBULAR NEURITIS
- Clinical Presentation
- Develops over hours and resolves over days, usually post-viral
- May mimic infarct type symptoms
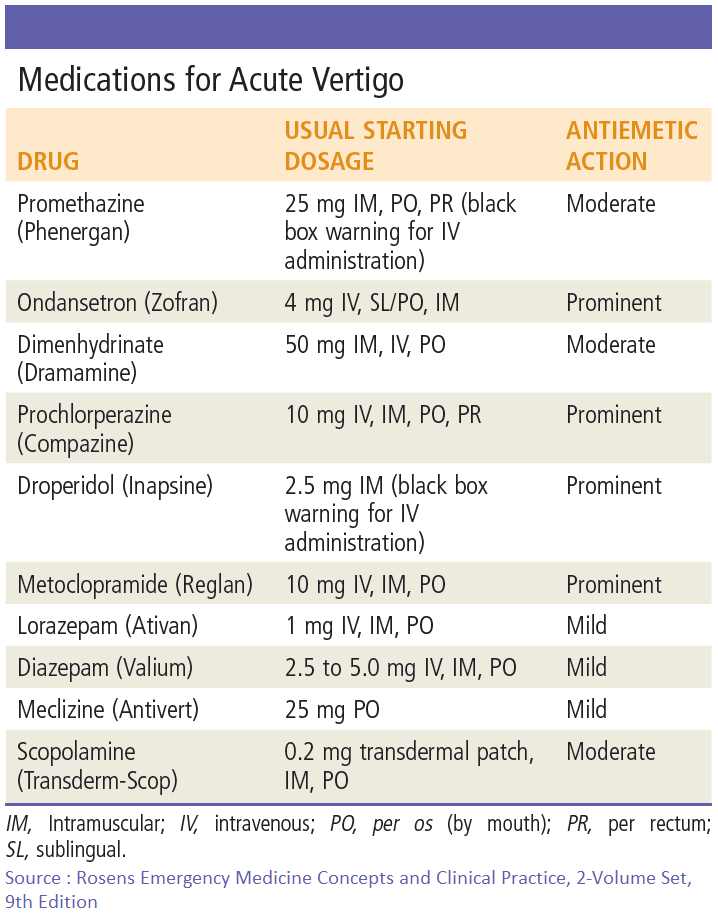
- Treatment
- General (Antihistamines, anticholinergics, anti-emetics, benzodiazepines)
- Directed treatment: Dexamethasone, valacyclovir
ACUTE LABYRINTHITIS
- Subtypes
- Toxic: usually medication induced, has auditory symptoms and tinnitus
- Serous: associated ENT infection, May have fever
- Suppurative: severe symptoms, febrile, toxic → Admit, IV Antibiotics, ENT C/S
LABYRINTHINE INFARCT
- Abrupt onset, h/o vascular dz, associated with neuro signs (also considered central type vertigo)
PERILYMPHATIC FISTULA
- Associated with trauma, lifting, coughing, sneezing
- Fistula test: Vertigo and nystagmus induced by pressure in the external ear canal
2. BPPV
Etiology
- Free floating debris in posterior semicircular canal
Clinical
- Abrupt onset of vertigo seconds after change in head position, lasting less than a minute.
Diagnosis
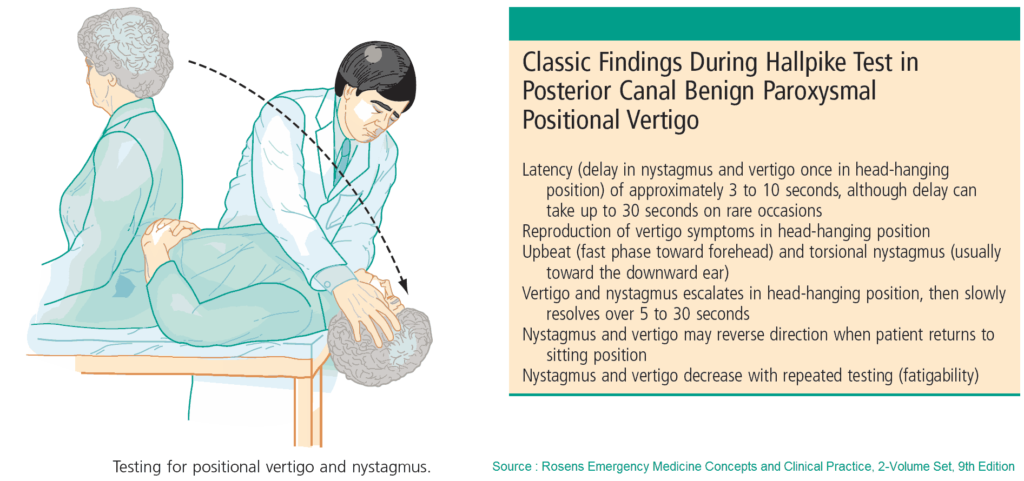
- Dix-Hallpike
- Use: for diagnosis, presence of paroxysmal positional nystagmus is most reliable finding in patients with BPPV (Am J Otol 1995;16:806-10)
- Procedure:
- Start: Seated with head turned 45º to side being tested
- Motion: Quickly lower to supine position with head angled backward 45º off bed
- Test positive: Nystagmus with affected side down, can continue to Epley from this position for treatment
- Nystagmus is delayed in onset, fatiguable, and decreases with fixation
Treatment
- Canalith Repositioning Maneuvers
- Epley and Semont (Ann Emerg Med 2001;37:392-8)
- May not be better than standard medical therapy (J Emerg Med 2014;46(4):575)
- Epley and Semont (Ann Emerg Med 2001;37:392-8)
3. Meniere’s disease
- Clinical
- Attacks of vertigo preceded/accompanied by reduced hearing, tinnitus and pressure in ear
- Attacks followed by residual hearing loss
- Treatment
- Dietary restrictions (salt, caffeine, tobacco), Lasix, Betahistine, ENT referral
- Other causes of Peripheral Vertigo
- Ear canal foreign body, trauma (labyrinth concussion), otitis media, cerumen impaction, medication (aminoglycosides)
Central Vertigo
Cerebellar Stroke
Clinical Scenario
- Symptoms
- Sudden onset/continuous vertigo
- +/- Severe headache
- Nystagmus
- Vertical, unilateral, nonfatigable, unsupressed
- Skew deviation
- Neurologic symptoms
- 5Ds (Dizziness, Dysphagia, Dysphonia, Dysmetria, Diplopia)
- Long tract signs (motor/sensory)
- Ataxia (unable to ambulate)
- Isolated vertigo
- Definition: no other symptoms present except for vertigo
- May simulate symptoms of vestibular neuritis (VN)
- Cerebellar CVA vs VN (Neurology 2006;67:1178-83)
- 10% isolated cerebellar infarct pts present with isolated vertigo symptoms (vestibular neuritis (VN) symptoms)
- No patients with cerebellar infarct had a positive head thrust test
Caution
10% isolated cerebellar infarct patients present with isolated vertigo
Diagnosis
- CT
- Can identify acute hemorrhage
- Not sensitive for acute stroke (especially of posterior fossa)
- Can identify large posterior CVA or mass effect (closed 4th ventricle)
- MRI
- Modality of choice to rule out infarctions
- Indication: (NEJM 1998;339:680-5)
- Neurologic signs/symptoms
- Sudden onset of vertigo in a patient with risk factors for stroke
- Headache: new, severe headache accompanying the vertigo
MRI for Vertigo
□ Neurologic symptoms
□ Sudden onset of vertigo + stroke risk factors
□ Headache: new and severe