Table of Contents
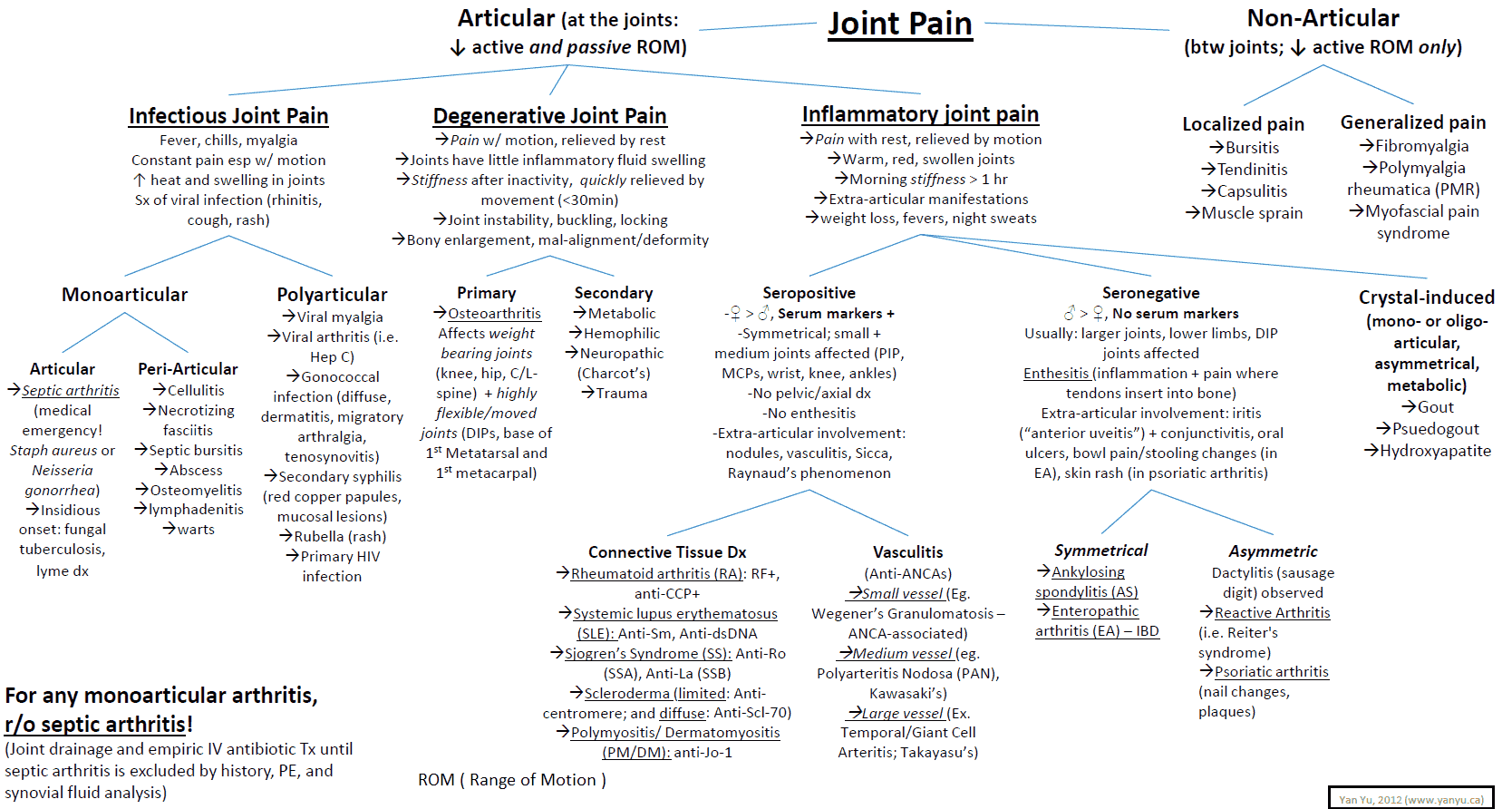
Differential Diagnosis of Joint Disease
It is important to distinguish accurately cases that need emergent care. These include:
- hot/swollen joints
- associated systemic symptoms (e.g., weight loss, malaise)
- neurologic symptoms
- weakness.
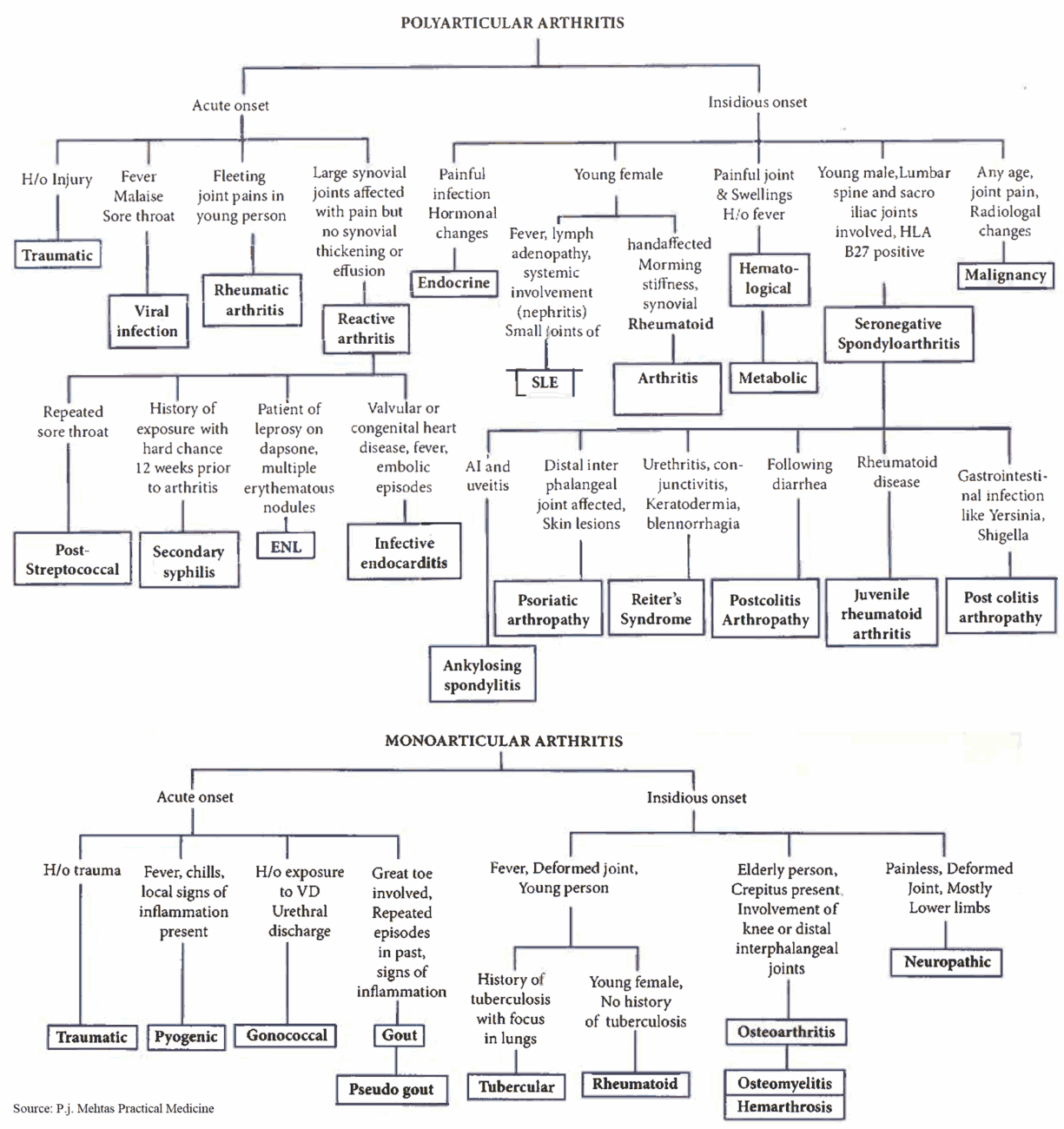
Common Causes of Joint Disease
- Rheumatoid arthritis (RA)
- Osteoarthritis (OA)
- Gout
- Seronegative arthritides: ankylosing spondylitis, Reiter’s syndrome, and psoriatic arthritis
- Septic arthritis
The causes of a single, hot, red joint are as follows:
- Septic arthritis, possibly secondary to rheumatoid arthritis, osteoarthritis, osteomyelitis, or injury
- Trauma
- Gout
- Pseudogout
- Hemarthrosis
- Gonococcal arthritis
- Rheumatoid arthritis
Less Common Causes of Joint Disease
- Enteropathic arthropathies (e.g., inflammatory bowel disease, Whipple’s disease).
- Behçet’s syndrome.
- Leukemia and lymphoma.
- Metastases: bronchial, breast, thyroid, kidney, and prostate carcinomas.
- Hypertrophic pulmonary osteoarthropathy: bronchial carcinoma.
- Viral, bacterial, and fungal infections.
- Endocrine causes: acromegaly, myxedema, hyperparathyroidism, idiopathic hyperparathyroidism.
- Metabolic diseases: Wilson’s disease, hemochromatosis, chondrocalcinosis, ochronosis, pyrophosphate arthropathy.
- Psychiatric causes: fibromyalgia, depression.
- Others: familial Mediterranean fever, sarcoidosis, amyloidosis, sickle cell disease, Wegener’s granulomatosis.
The causes of joint pain can be remembered by the mnemonic SOFTER TISSUE: sepsis, osteoarthritis, fractures, tendon/muscle, epiphyseal, referred, tumor, ischemia, seropositive arthritides, seronegative arthritides, urate, extra-articular rheumatism (e.g., polymyalgia).
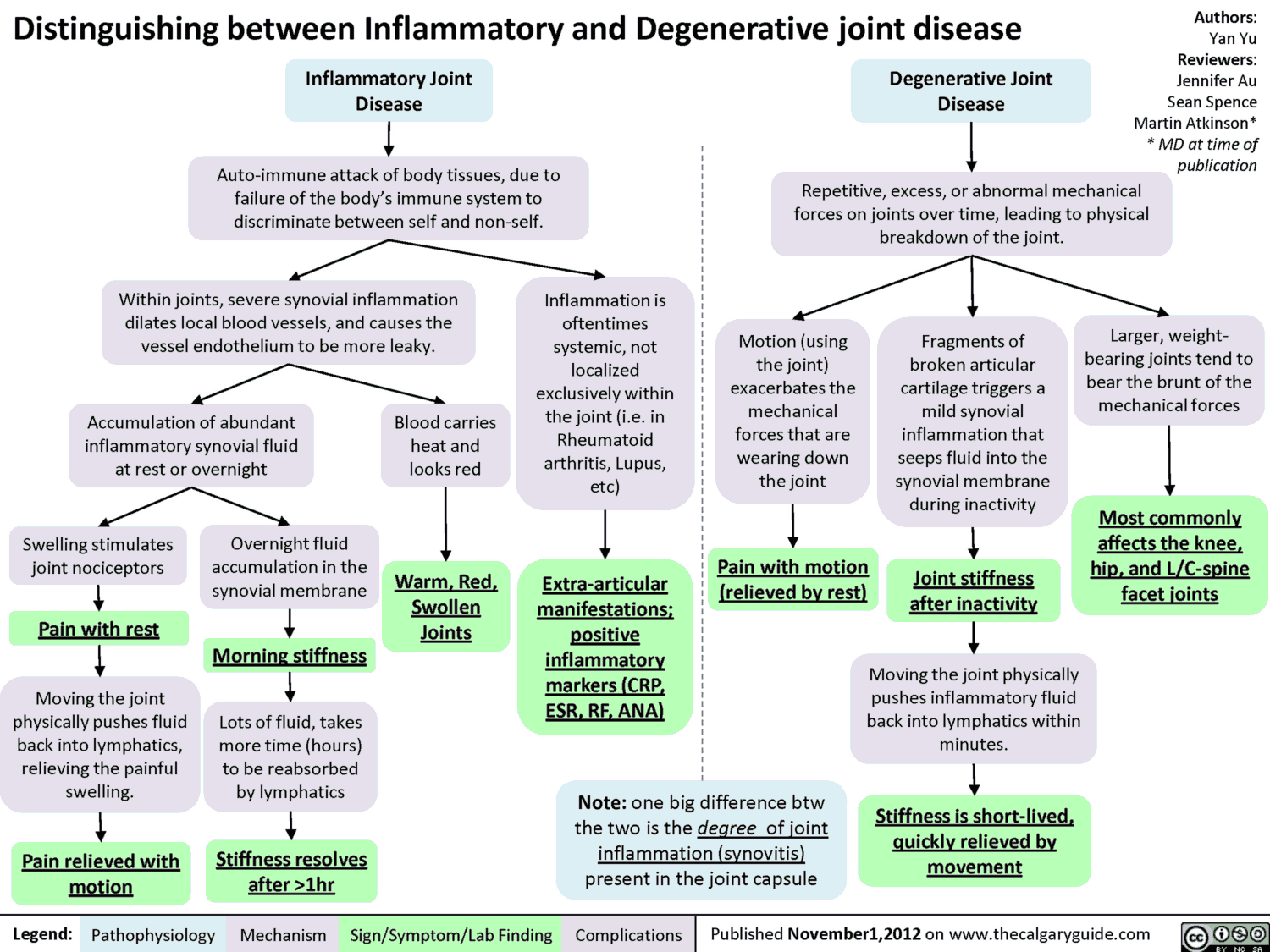
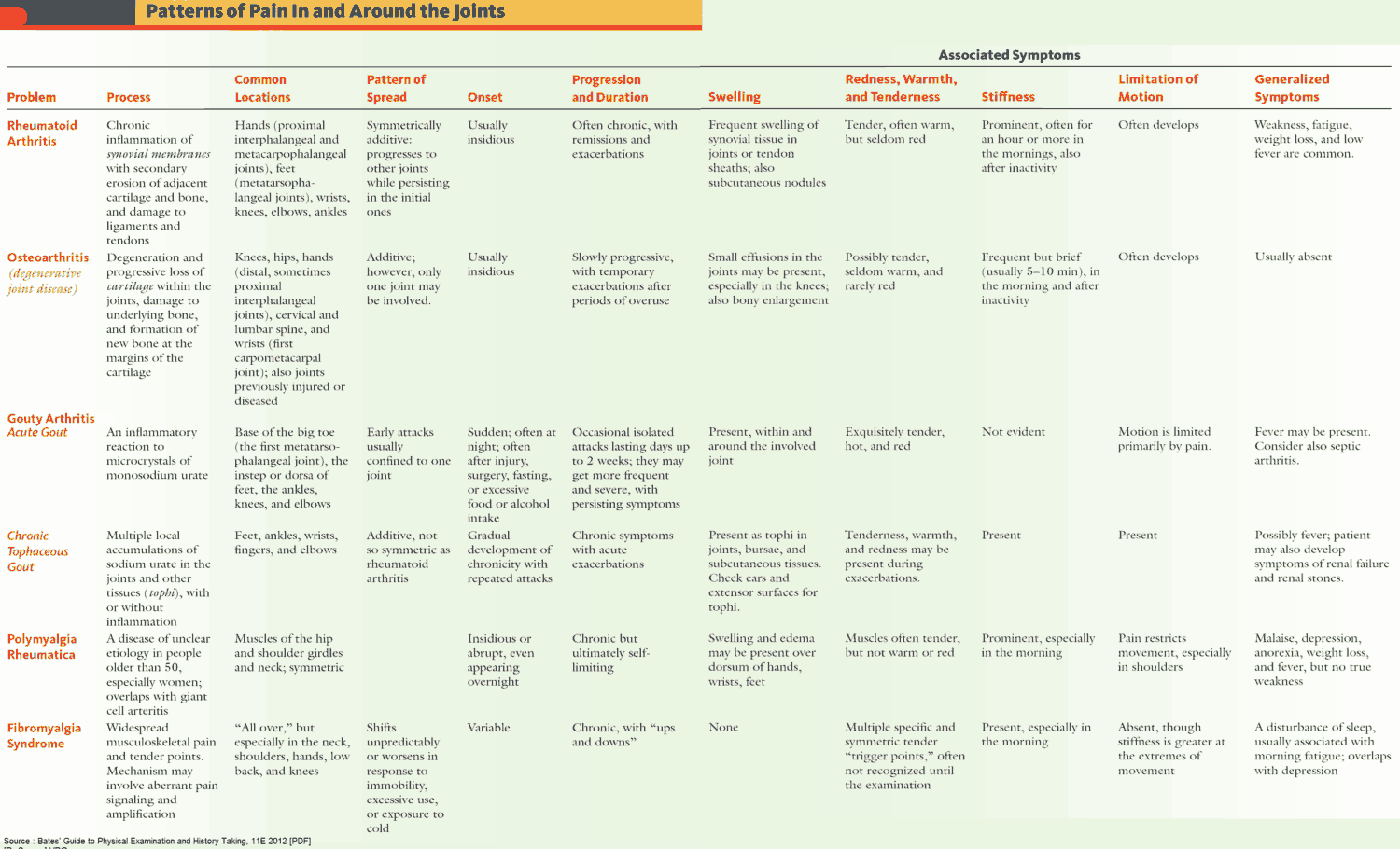
History in the Patient with Joint Disease
The different types of joint disease have many features in common, and examination will provide further additional important clues to the etiology. Ask about the following:
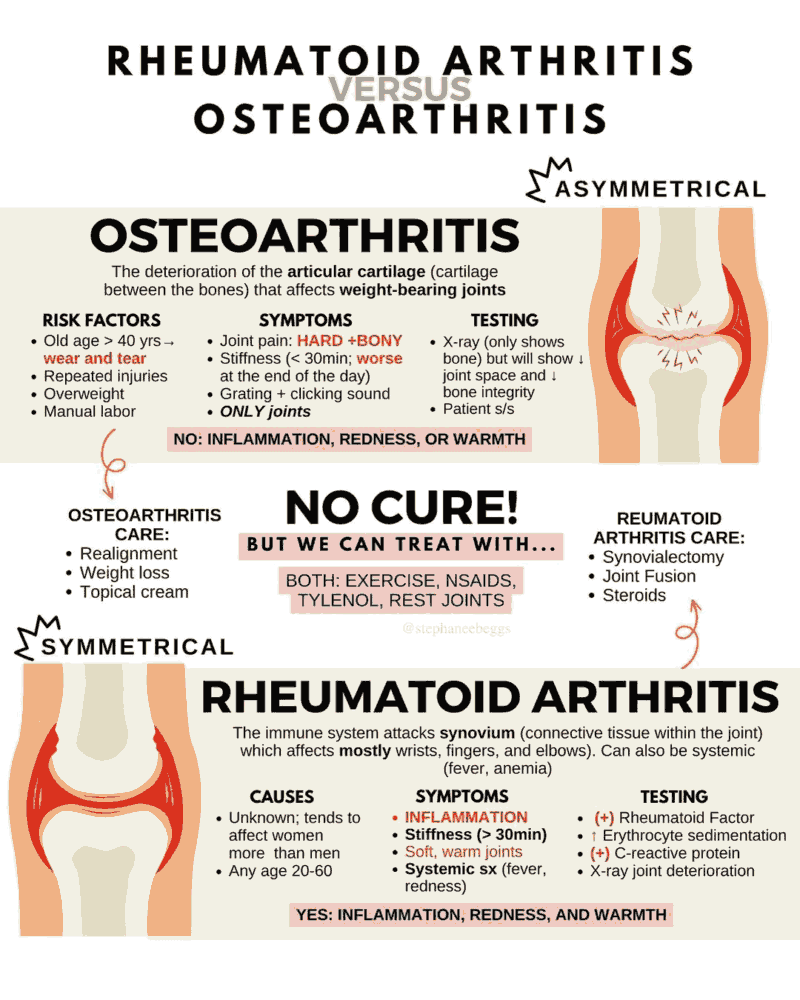
- Onset: rapid or slowly progressive.
- Persistent or relapsing. Gout has a classic history of recurrent attacks or inflammation.
- Association with movement. OA improves with movement and worsens with rest.
- Early morning stiffness: classically RA is worse first thing in the morning and OA is worse at the end of the day, although there is considerable overlap.
- Weakness: with or without wasting of muscles.
- Distribution of the affected joints, monoarticular vs. polyarticular (see below).
- Patient’s age: RA classically affects women aged 25-55 years, and OA usually occurs in patients over 40.
- Any history of trauma.
- Drug history: procainamide, hydralazine, isoniazid, and methydopa can cause a lupus-like syndrome; thiazide diuretics cause a predisposition for gout.
- Recent infection (e.g., viral illness and reactive arthritis, septic arthritis, or neutropenia).
- Features associated with different arthropathies: inflammation of the eye (RA and seronegative arthropathies), shortness of breath (fibrosis or aortic regurgitation in RA, and ankylosing spondylitis), paresthesias (entrapment neuropathies), gastrointestinal symptoms (enteropathic arthropathies), and rarer causes of arthropathies (e.g., endocrine causes).
- In patients with chronic arthritis it is important to explore the extent of loss of function. How limited are the activities of daily living?
- Chronic arthritis can lead to feelings of helplessness and depression. Assessment of these features is also an important part of the history.
Examination and Signs in the Patient with Joint Disease
Remember: “Look, feel, move, and measure”:
- Look: inspect for joint swelling, redness, muscular atrophy.
- Feel: palpate for warmth, joint effusion, and tenderness.
- Move: move the joint passively and ask the patient to move the joint actively. Look for limitation in the range of motion, tenderness, and joint subluxation.
- Measure: use a tape measure to determine muscular atrophy of large joints or decrease in size of limbs, etc.
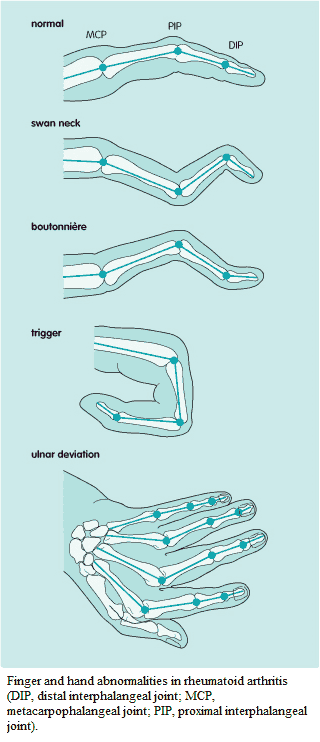
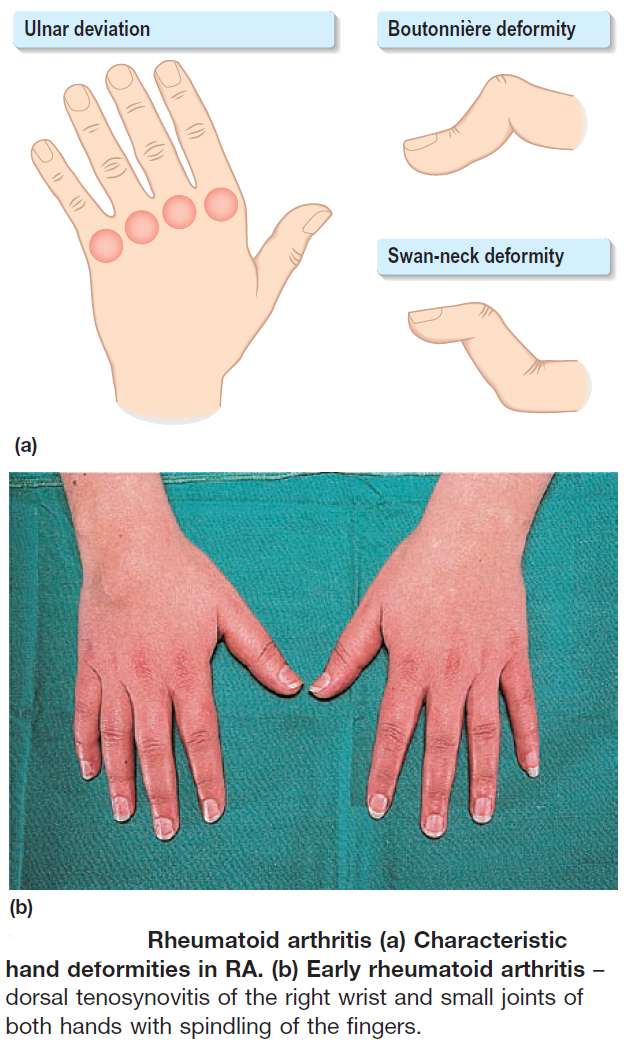
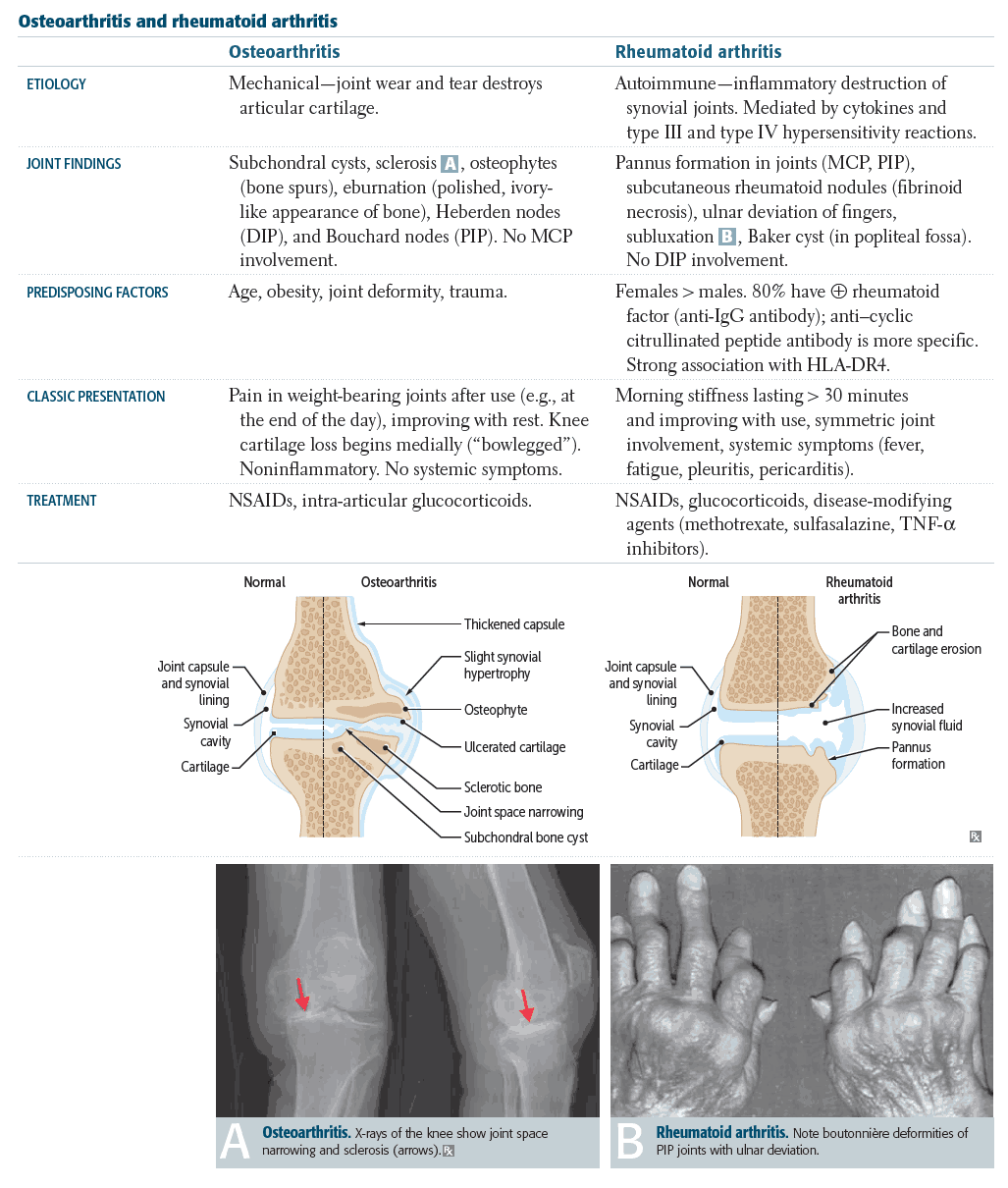
Examination and Signs in Rheumatoid arthritis
RA is a systemic connective tissue disorder, the joints being one of many body parts affected. Look for the following:
- Symmetrical deforming arthropathy.
- Swelling of the proximal interphalangeal (PIP) and metacarpophalangeal (MCP) joints.
- For diagnosis, swelling must be present in 3 or more joints for 6 weeks.
- Wasting of the small muscles of the hand.
- Nodules on the elbows and extensor tendons. They are nonfixed and several millimeters in diameter.
- Ulnar deviation of the fingers: subluxation and dislocation at the MCP joints.
- Swan neck deformity: hyperextension of the PIP joints and flexion of the MCP and distal interphalangeal (DIP) joints.
- Boutonnière deformity: flexion of the PIP joints and extension of the DIP and MCP joints.
- Swollen or deformed knees.
- Cervical spine disease.
- Anemia due to:
- Normochromic normocytic anemia of chronic disease.
- Microcytic anemia from chronic blood loss secondary to drug treatment.
- Bone marrow suppression from treatment (e.g., gold or penicillamine).
- Megaloblastic anemia from impaired folate release or pernicious anemia.
- Felty’s syndrome.
- Systemic symptoms: weight loss, malaise, low-grade fever, depression. Usually on acute presentation.
- Arteritic lesions: nail-fold infarcts, chronic leg ulceration, and purpuric rash.
- Determine how the joint disease affects the patient’s daily activities (e.g., holding a pan, making a cup of tea).

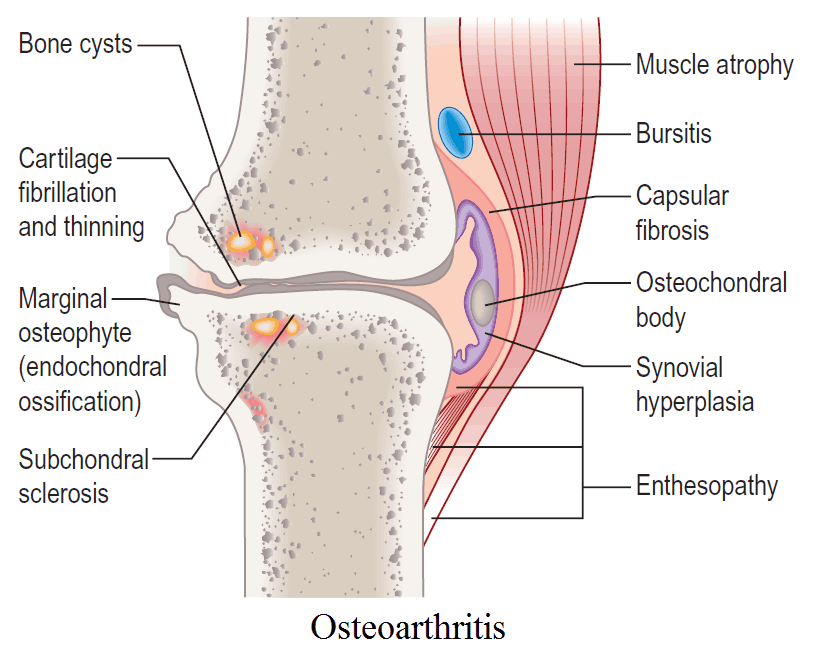
Examination and Signs in Osteoarthritis
In the hands in OA look for the following:
- Heberden’s nodes: swelling of the DIP joints.
- Bouchard’s nodes: swelling of the PIP joints.
- Subluxation of the first metacarpal: square hand appearance.
- Crepitus of affected joints.
- Hip pain: common in patients with OA.
- Wasting and weakness of the quadriceps and glutei.
- Positive Trendelenburg’s sign: this is a downward tilting of the pelvis when the patient stands on the affected leg.
- Joint effusions.
- Loss of function.
Examination and Signs in Gout
Look for the following:
- Asymmetrical swelling of the small joints of the hand and feet.
- Tophi: look especially on the helix of the ear and tendon sheaths.
- Look for associations: hyperlipidemia (xanthalasmata and corneal arcus), hypertension, signs associated with diabetes mellitus.
Examination and Signs in Seronegative Arthritides
Ankylosing spondylitis
Ask the patient to sit or stand up. Look for the following:
- Loss of lumbar lordosis and a fixed kyphosis.
- A stooped “question mark” posture.
- Rigid spine.
- Reduced chest expansion.
- Prominent abdomen.
- Also examine for complications and extra-articular manifestations:
- Eyes: iritis.
- Cardiovascular system: aortitis (listen for aortic regurgitation and conduction defects).
- Chest: apical fibrosis.
- Neurologic: atlantoaxial dislocation leading to paraplegia or sciatica.
Reiter’s syndrome
This is a triad of urethritis, conjunctivitis, and seronegative arthritis. It follows nonspecific urethritis or occasionally dysentery. Look for the following:
- Large joint mono- or oligoarthritis.
- Iritis.
- Keratoderma blenorrhagica (brown, aseptic abscesses on the soles and palms).
- Mouth ulcers.
- Circinate balanitis.
- Enthesopathy (plantar fasciitis or Achilles tendinitis).
- Aortic regurgitation.
Psoriatic arthritis
- Asymmetrical arthropathy.
- Usually involvement of the DIP joints.
- Pitting of the fingernails and onycholysis.
- Thickened nails.
- Psoriatic plaques: look particularly at the elbows, extensor aspects of limbs, scalp, behind the ears, and the navel.
- Other forms of psoriatic arthropathy: arthritis mutilans, a RA-like picture, asymmetrical mono- or oligoarthropathy, ankylosing spondylitis.
Examination and Signs in Septic Arthritis
This must be recognized and treated promptly because of potential destruction of the joint and widespread infection. It usually presents as a monoarthritis. The affected joint is swollen, painful, hot, and red.
You must also carry out a general examination. In particular, look for the following:
- Eye signs: keratoconjunctivitis sicca, keratitis, episcleritis, scleromalacia perforans, cataracts due to chloroquine or steroids.
- Dry mucous membranes: Sjögren’s syndrome.
- Chest signs: pleural effusion, fibrosing alveolitis.
- Neurologic signs: peripheral neuropathy, mononeuritis multiplex, entrapment neuropathy.
- Vasculitic leg ulceration.
- Felty’s syndrome: splenomegaly, neutropenia.
- Cardiac signs: pericarditis, myocarditis, conduction defects, and valvular incompetence.
- Secondary amyloidosis.
- Other autoimmune disorders.
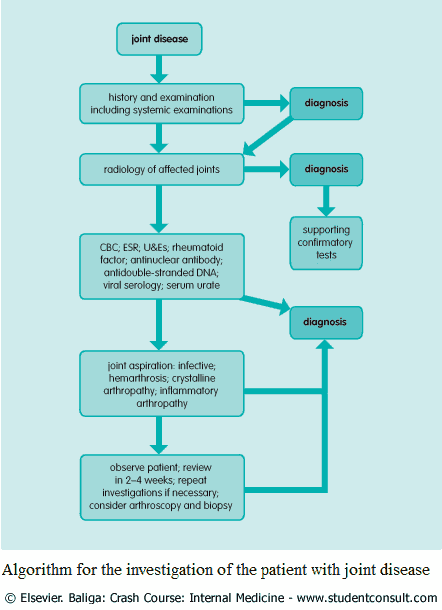
Investigation and Diagnosis in the Patient with Joint Disease
- Complete blood count:
- anemia
- raised white cell count occasionally in RA
- leukopenia and thrombocytopenia in SLE
- eosinophilia in PAN
- neutropenia in Felty’s syndrome
- Erythrocyte sedimentation rate/C-reactive protein: nonspecific but raised in the presence of inflammation (therefore often high in RA but less so in OA).
- Rheumatoid factor: positive in about 75% of patients with RA. It may also be positive in SLE, mixed connective tissue diseases, scleroderma, Sjögren’s syndrome, and viral illnesses.
- Antinuclear antibodies: positive in 30% of patients with RA and in 80% of patients with SLE.
- Anti-double-stranded DNA antibodies: high titers in SLE.
- Other autoantibodies according to clinical suspicion (e.g., anti-Ro and anti-La antibodies in Sjögren’s syndrome and anti-Scl70 antibodies in scleroderma).
- Viral serology: if a viral cause for the arthropathy is suspected (e.g., rubella, mumps, infectious mononucleosis, coxsackie virus, and hepatitis B virus).
- Urea and electrolytes: associated renal involvement.
- Liver function tests: liver involvement or drug treatment.
- Creatine phosphokinase: myositis.
- Serum urate: usually high in gout but beware of false positives and false negatives.
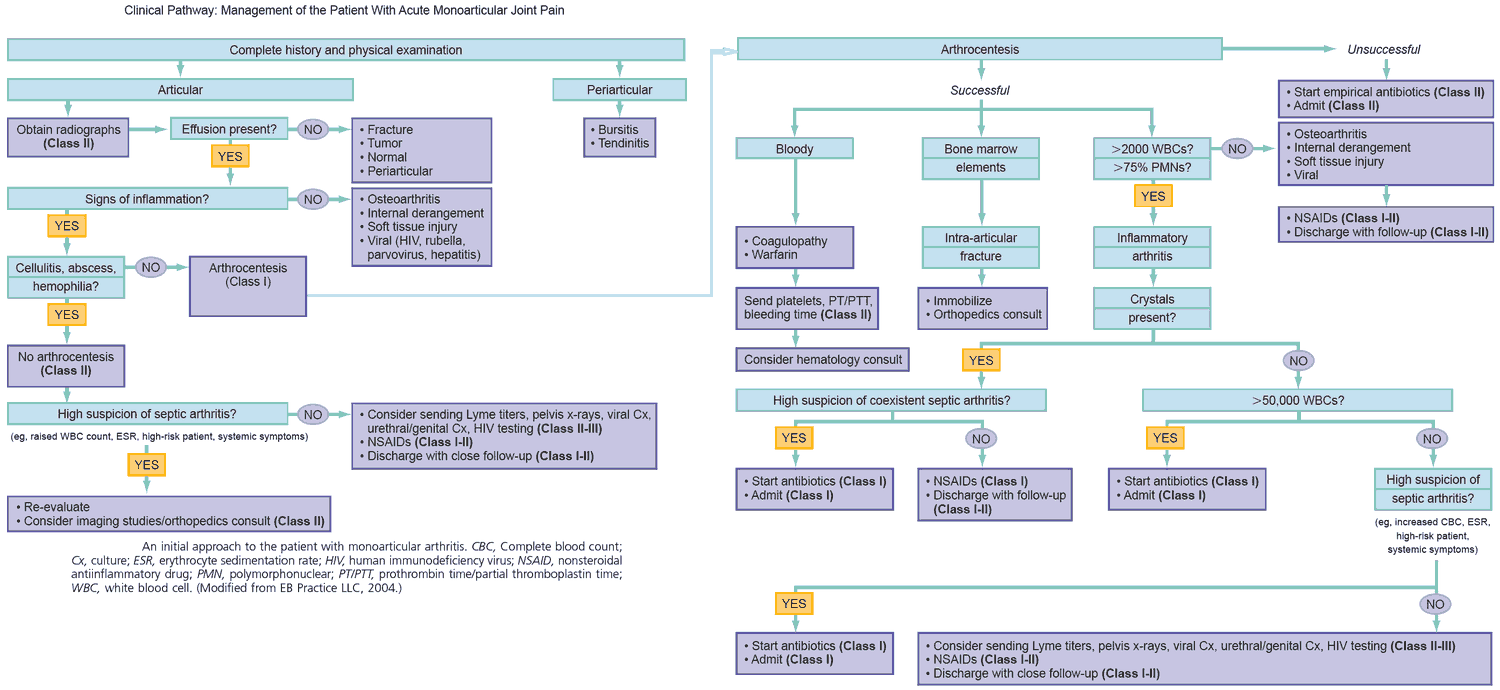
- Joint aspiration should be performed. Examine the following:
- Appearance: purulence indicates infection, frank blood indicates hemarthrosis or traumatic tap.
- Microscopy for bacteria and crystals: monosodium urate indicates gout, calcium pyrophosphate indicates pseudogout.
- In pseudogout, crystals are positively birefringent in plane-polarized light. Remember this by the “Ps.” In gout, the crystals are negatively birefringent.
- White cell count: high in inflammatory arthropathies.
- Culture: gonococci, tubercle bacillus, or fungi when indicated.
- A chest x-ray should be performed to look for associated diseases or complications of RA:
- Pleural effusion.
- Diffuse fibrosing alveolitis.
- Rheumatoid nodules or cavities.
- Cricoarytenoid arthritis.
- Obliterative bronchiolitis.
- Rheumatoid pneumoconiosis: Caplan’s syndrome.
- An x-ray of the affected joints may indicate the following:
- RA: soft tissue thickening, juxta-articular osteoporosis, loss of joint space, bony erosions, subluxation.
- OA: loss of joint space, subchondral sclerosis and cysts, marginal osteophytes.
- Gout: soft tissue swelling and punched-out lesions in juxta-articular bone.
- Ankylosing spondylitis: “bamboo spine” (squaring of the vertebrae and obliteration of sacroiliac joints); also found in Reiter’s syndrome and Crohn’s disease.
- An x-ray of the cervical spine should also be used to look for displacement of the odontoid peg.
- Arthroscopy allows direct visualization inside the joint space, and can be used for biopsy and the removal of foreign bodies.