Table of Contents
Epidemiology of Sarcoidosis
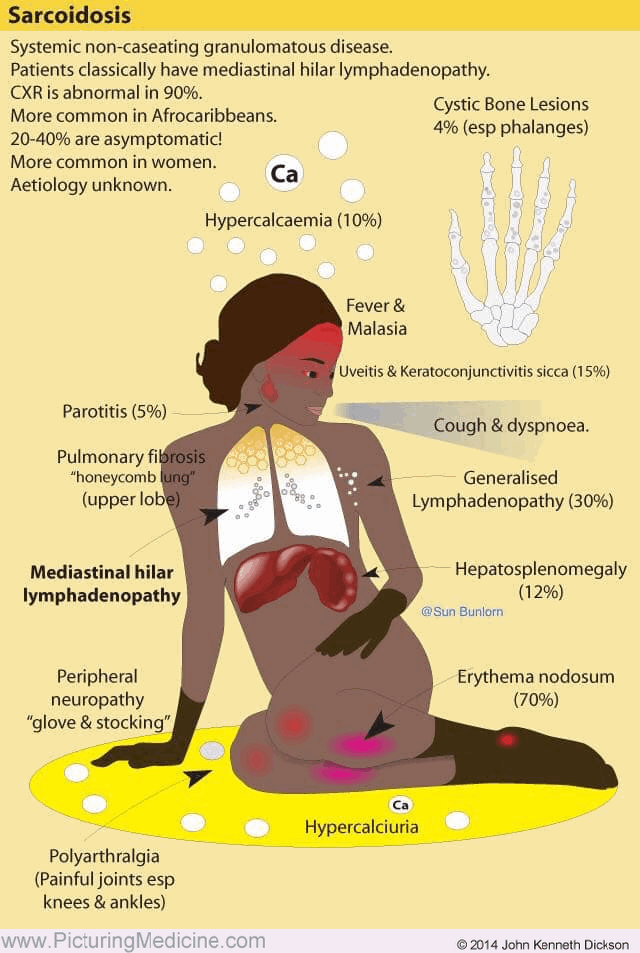
Sarcoidosis has a worldwide prevalence of 10 to 20 per 100,000. The etiology and pathogenesis of this disease remain unknown. African Americans have a 3% higher lifetime risk and present an average of 10 years earlier with symptoms, and symptoms are more acute compared to Caucasians.
Symptoms and Signs of Sarcoidosis
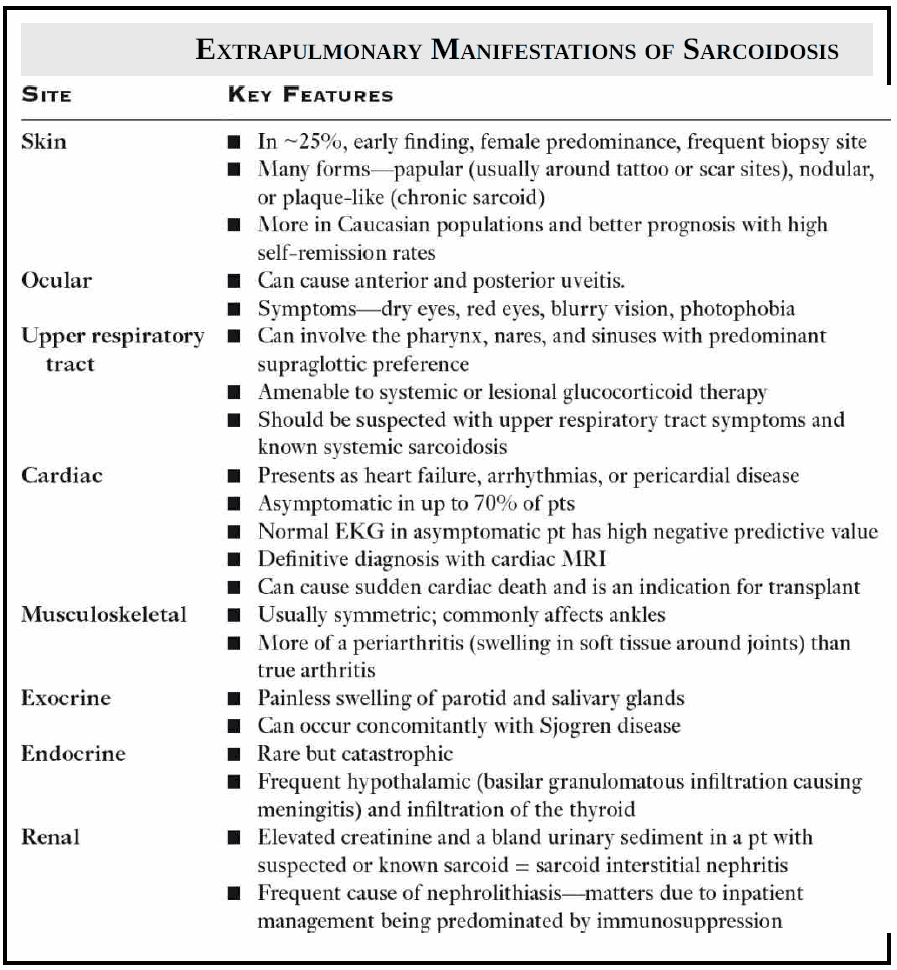
Ultimately, sarcoidosis is a multisystem granulomatous disorder that is characterized by noncaseating granulomas. Pulmonary involvement is the most common manifestation, but extrapulmonary manifestations are seen in up to 30% of patients.
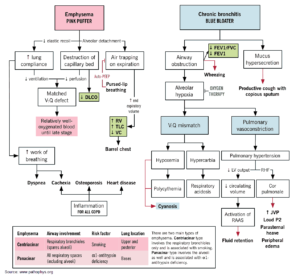
Extrapulmonary manifestations of sarcoidosis are crucial to define the extent of disease and often provide safer biopsy options during the diagnostic workup. Extrapulmonary symptoms of sarcoidosis are listed in the image bellow.
Clinical suspicion should be raised if one or more of the following are present:
- bilateral hilar adenopathy
- pulmonary reticular opacities
- skin or eye lesions
Diffuse interstitial lung disease is the most common pulmonary presentation. Symptom onset is generally between the ages of 20 and 60 years and includes:
- cough
- chest pain
- dyspnea
Older patients may present with more subtle symptoms of dyspnea but have a greater proportion of fatigue and weight loss.
Evaluation and Diagnosis of Sarcoidosis
Radiographic abnormalities
Radiographic abnormalities often are detected before clinical and physical exam findings. The most common radiographic progression of disease is:
- initial hilar adenopathy with possible subsequent regression
- upper lung reticular opacities
- volume loss
- eventual traction bronchiectasis.
High-resolution Chest Computed Tomography (HRCT)
High-resolution chest computed tomography (HRCT) is the next step in the evaluation of a patient with marked dyspnea, cough, and a suspicious radiograph for sarcoidosis. HRCT helps to determine the extent of parenchymal disease and to exclude other crucial diagnoses.
Pulmonary Function Tests (PFTs)
The next step in the evaluation of patients with suspected sarcoidosis is referral to pulmonary medicine for outpatient pulmonary function tests (PFTs) and a 6-minute walk test.
PFTs reveal a restrictive lung pattern and decreased:
- vital capacity (VC)
- total lung capacity (TLC)
- diffusion of carbon dioxide
Biopsy of the Pulmonary Lesions
Ultimately, biopsy of the pulmonary lesions is needed to confirm the diagnosis. One major exception is Lofgren syndrome. This presents with fever, arthralgias, erythema nodosum, and bilateral hilar lymphadenopathy. The presence of all features of Lofgren syndrome has been shown to have a 95% specificity for sarcoidosis, as biopsies in the setting of this syndrome have a high false-negative rate.
Therapy of Sarcoidosis
Glucocorticoid Therapy
Therapy is based on the extent of pulmonary and extrapulmonary involvement. While glucocorticoid therapy is the primary therapy for pulmonary sarcoidosis, adjunctive therapy with nonglucocorticoids is also indicated in certain cases.
The main therapeutic considerations for the emergency provider are when to initiate steroid therapy with steroids and at what dose and duration of therapy. Most patients with pulmonary sarcoidosis do not require therapy in the emergency department, as many are asymptomatic and have a high rate of spontaneous remission.
Steroid therapy is not indicated for stage I disease and for most patients with stable stage II or III disease due to the side effects of steroid therapy.
Initiation of steroid therapy is indicated for patients with debilitating symptoms and worsening radiographic finding combined with declining pulmonary function. The intent of steroid therapy is to prevent irreversible pulmonary fibrosis.
Highdose steroid therapy (80 to 100 mg daily) may be indicated for cardiac, neurologic, ocular, or upper airway disease. Emergency providers should also consider adrenal insufficiency as an etiology of symptoms in sarcoidosis patients with steroid medication noncompliance or temporary inability to tolerate medications.
In general, short-term steroid therapy is not sufficient, as most patients should be initiated on 0.3 to 0.6 mg/kg/d (ideal body weight) for 6 weeks. Prompt consultation with the patient’s pulmonologist should be considered to coordinate care and follow-up evaluation.
Other immunosuppressive agents
Other immunosuppressive agents are considered in the patient who is unable to tolerate steroid side effects, failed to wean from long-term steroids, and failed to respond despite an adequate dose of steroids. The most commonly used agents include:
- methotrexate
- leflunomide
- tumor necrosis factor-α antagonists (Remicade)
- azathioprine
- antimalarial agents.
The initiation of such adjunctive therapy should not occur in the emergency department.
Key Points
- Consider sarcoidosis in the patient with cough, dyspnea, and hilar lymphadenopathy.
- Extrapulmonary manifestations are seen in up to 30% of patients with sarcoidosis.
- Consider other etiologies of hilar lymphadenopathy such as human immunodeficiency virus infection, occupational or environmental exposure, mycobacterium infections, fungal infections, pneumoconiosis, and hypersensitivity pneumonitis.
- Noncaseating granulomas are the hallmark of sarcoidosis.
- Initiate appropriate steroid therapy for debilitating symptoms, worsened radiographic opacities with increased pulmonary function impairment. Start with 0.3 to 0.6 mg/kg/d (ideal body weight) of prednisone.