The evaluation of the emergency department (ED) patient with acute chest pain centers on the history of present illness (HPI), physical examination, and electrocardiogram (ECG). Often, the emergency provider (EP) utilizes troponin values and the results of prior cardiac stress tests to further risk stratify patients and determine the need for additional management.
The role of prior cardiac stress tests in the risk stratification of ED patients with suspected acute coronary syndrome (ACS) is uncertain.
Goal of a cardiac stress test
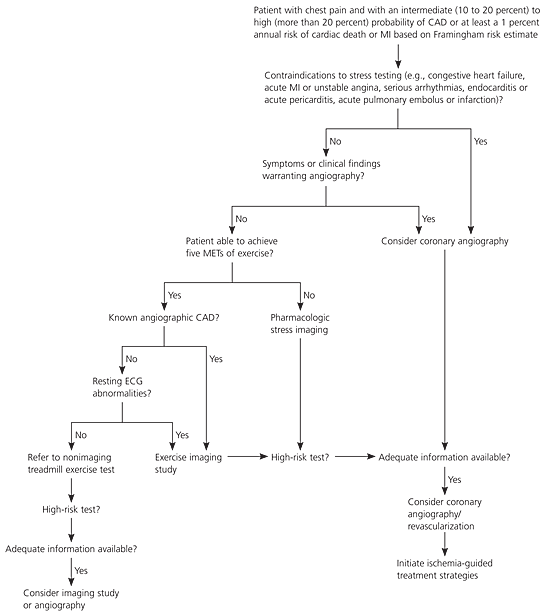
The goal of a cardiac stress test is to identify the patient with obstructive coronary artery disease (CAD), typically defined as stenosis of 50% or more of a coronary artery on angiography.
Types od Cardiac Stress Tests
Traditional stress tests include:
- exercise ECG (on a treadmill),
- echocardiography
- nuclear medicine studies
All have rest and exercise phases. The exercise phases of echocardiography and nuclear medicine studies can be performed with physical exertion or chemically induced with medication such as adenosine or dobutamine.
Depending on the study, the test will detect ischemic ECG changes, wall motion abnormalities, or diminished tracer update indicative of decreased perfusion to regions of the myocardium. Test availability, the patient, and the presence of comorbid conditions often determine the type of stress test that is performed.
Sensitivity and Specificity of Cardiac Stress Tests
The pooled sensitivity for all cardiac stress tests range from 67% to 85%, with specificity that ranges from 70% to 95%. Stress tests have higher sensitivity in patients with multivessel CAD.
Exercise ECG stress tests have a sensitivity of 68% and a specificity of 77% for CAD. The presence of multivessel disease increases the sensitivity to 81%. Importantly, the sensitivity and specificity are lower in women than in men. Most cardiologists obtain an exercise ECG stress test as the initial outpatient test.
Recently, coronary computed tomography angiography (CCTA) has emerged as a means of diagnosing CAD and defining coronary lesions. The pooled sensitivity of CCTA ranges between 98% and 99%, with a specificity between 82% and 89%. The positive predictive value of CCTA is reported to be 85%, whereas the negative predictive value is ~92%.
The ED patient with acute chest pain is very different from the asymptomatic patient who undergoes a routine outpatient cardiac stress test.
Nerenberg and colleagues reviewed the disposition of ED patients evaluated for ACS. The authors found that a previous negative stress test did not change the rate of hospital admission. Furthermore, there was no difference in the rate of adverse events among patients with a positive stress test, a negative stress test, or no previous stress test.
In another series of ED patients, Smith and associates found that ~5% of patients were diagnosed with an acute myocardial infarction within 3 years of a negative stress test result.
Walker and colleagues reviewed the records of ED patients with chest pain and a negative, or inconclusive, stress test result within the preceding 3 years. This study included treadmill and pharmacologic echocardiograms, pharmacologic nuclear medicine studies, treadmill nuclear studies, and a treadmill ECG-only evaluation. The authors defined CAD as a myocardial infarction identified by positive cardiac enzymes, a subsequent positive stress test, a cardiac catheterization that required intervention, coronary artery bypass graft surgery, or death caused by cardiac arrest. Approximately 20% of patients were diagnosed with CAD after a negative stress test within 3 years of the ED presentation. Of patients with significant CAD, 23.5% had a negative stress test within 1 month before their ED presentation.
Cardiac stress test is a valuable tool for cardiologists to screen outpatients for CAD. In an outpatient setting, stress tests are used to identify fixed obstructions to coronary artery flow.
In ED patients with acute chest pain, however, the intent of testing is to identify acute plaque rupture and thrombus formation. As such, cardiac stress tests have limited utility in the ED evaluation of acute chest pain.
The EP should not exclude an ACS in the ED patient with acute chest pain based solely on a recent negative stress test result. If the HPI is concerning, the EP should continue with the evaluation and subsequent admission.
Key Points
- Cardiac stress tests have a pooled sensitivity of 67% to 85%.
- The sensitivity of stress tests is higher in patients with multivessel disease than in those with single-vessel disease.
- The sensitivity and specificity of exercise ECG stress testing are lower in women than in men.
- A previous negative stress test should not be the basis for subsequent decisions regarding hospital admission.
- Significant CAD can be present despite a recent negative stress test result.
Suggested Readings
- Arbab-Zadeh A. Stress testing and non-invasive coronary angiography in patients with suspected coronary artery disease: Time for a new paradigm. Heart Int. 2012; 7(1):e2. https://pubmed.ncbi.nlm.nih.gov/22690295/
- Gibbons RJ, Balady GJ, Bricker JT, et al. ACC/AHA 2002 guideline update for exercise testing: Summary article: A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2002;106(14): 1883–1892. https://pubmed.ncbi.nlm.nih.gov/12356646/
- Nerenberg RH, Shofer FS, Robey JL, et al. Impact of a negative prior stress test on emergency physician disposition in ED patients with chest pain syndromes. Am J Emerg Med. 2007;25(1):39–44. https://pubmed.ncbi.nlm.nih.gov/17157680/
- Smith SW, Jackson EA, Bart BA, et al. Incidence of myocardial infarction in emergency department chest pain patients with a recent negative stress imaging test. Acad Emerg Med. 2005;12(5):51.
- Walker J, Galuska M, Vega D. Coronary disease in emergency department chest pain patients with recent negative stress testing. West J Emerg Med. 2010;11(4): 384–388. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2967694/

![Read more about the article Atrial Flutter: ECG Interpretation [With Examples]](https://manualofmedicine.com/wp-content/uploads/2022/01/Atrial-Flutter-with-4-1-AV-Block-300x135.png)
![Read more about the article Conduction Blocks at the AV Node (AV Blocks) [With Examples]](https://manualofmedicine.com/wp-content/uploads/2021/05/Excerpt-AV-Blocks-300x243.jpg)