Table of Contents
Acute mesenteric ischemia (AMI) occurs when blood flow to the small intestines is not sufficient for normal bowel function. AMI is a high-risk diagnosis that carries an extremely high mortality rate (beyond 70%) if not recognized in a timely manner before bowel infarction occurs.
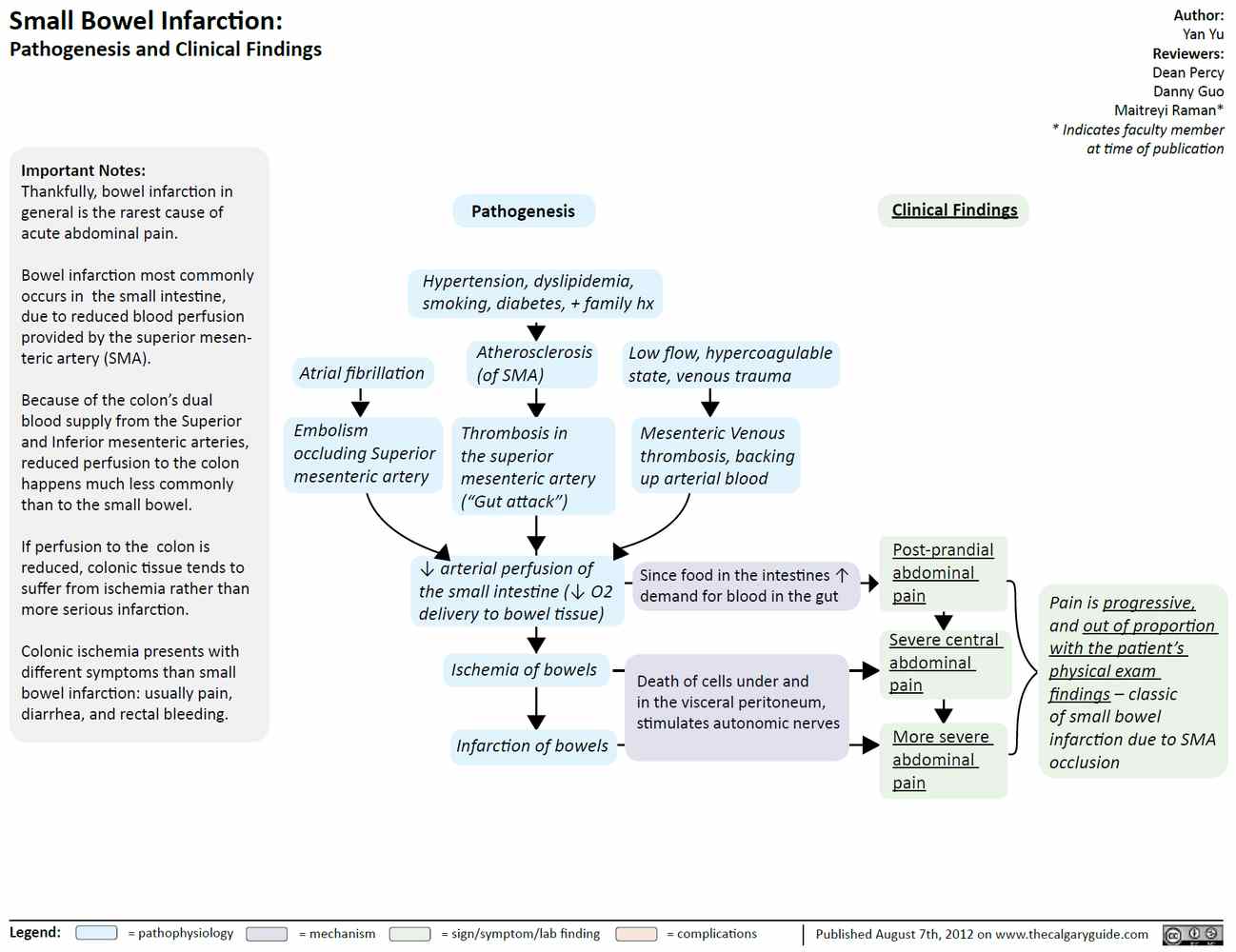
AMI can be divided into three different syndromes based on pathophysiology. It is important to distinguish these, as each one has different risk factors and different management strategies :
- Acute mesenteric arterial occlusion is the most common (65% to 70%) and the most devastating cause with the highest mortality. It is mostly commonly encountered in elderly patients. The majority of these cases result from embolization of clots from the heart. The main risk factors are atrial fibrillation and myocardial akinesis, for example, as seen in an acute myocardial infarction. The remaining cases of mesenteric arterial occlusion occur due to an in situ thrombotic event in patients with severe atherosclerosis, mostly at the site of the proximal SMA. As the mechanism resembles that of a myocardial infarction, the main risk factors similarly are age, hypertension, and severe vascular disease. About half of these patients endorse a history of postprandial abdominal angina.
- Mesenteric venous thrombosis (5% to 15%) is the only category of AMI that tends to affect younger patients. It has a similar mechanism as in other cases of venous thromboembolism (e.g., deep vein thrombosis and pulmonary embolism) and is likewise seen in patients with hypercoagulable states. In fact, the majority of patients with AMI have a history of deep vein thrombosis. While the mortality rate is lower than in the other categories of AMI, it is still high at about 20% to 50%.
- Nonocclusive mesenteric ischemia (20%) is a multifactorial condition often seen in hospitalized patients without evidence of a vascular occlusion. It can be caused by shock, a decrease in cardiac output, or medications (e.g., nodal blockers, vasoconstrictors) and can occur with or without narrowing of the mesenteric vasculature. It is associated with a high mortality, often due to the underlying condition.
Presentation of Acute Mesenteric Ischemia
The presentation of AMI varies based on the category, but the majority of patients complain of sudden onset of severe colicky, poorly localized abdominal pain that is often out of proportion to the examination findings.
However, we cannot rely on this classically taught presentation of AMI. One of the main pitfalls of AMI is that some patients may have a seemingly benign examination and may initially only complain of mild diffuse abdominal discomfort.
Abdominal distention and peritoneal signs are usually late findings that suggest that the bowel has already become necrotic. Septic shock and multiorgan dysfunction can develop well before, but bowel necrosis often occurs 10 to 12 hours after symptom onset. At this stage, mortality is about 70%.
Diagnosis of Acute Mesenteric Ischemia
Although often elevated, many laboratory studies like the white blood cell count, creatine kinase, phosphate, and amylase levels are neither sensitive nor specific enough to be helpful. An elevated lactate level has a good sensitivity; however, it may not pick up the early stages of the disease process, nor is it specific for AMI. Recently, the D-dimer assay has been promoted in the evaluation of AMI. Due to its high sensitivity, some authors suggest it could be utilized as a screening tool to rule out AMI.
The first-line imaging choice is CT angiography (CTA), though it only has a 12% to 15% sensitivity to directly visualize the lesion. Other CT findings include focal lack of bowel wall enhancement, bowel wall thickening, fat stranding, or pneumatosis intestinalis. Oral contrast should be avoided as it can obscure the view of the blood vessels. While CT is now considered first line given its availability, the gold standard remains conventional angiography for diagnosis and possibly therapy in the case of arterial occlusion.
Management of Acute Mesenteric Ischemia
Management includes intravenous (IV) fluid resuscitation, IV antibiotics, nasogastric tube placement, avoidance of nodal blockers and vasoconstrictive medications, and early surgical consultation. If vasopressors are needed for resuscitation, it is recommended that α-agonists be avoided.
If there is bowel necrosis on CT or peritoneal signs, immediate laparotomy is indicated, no matter the cause of ischemia.If no bowel necrosis is evident, specific management differs between the syndromes.
- If the cause is arterial occlusion, revascularization should be attempted with intra-arterial vasodilator infusion (e.g., papaverine) by interventional radiology or in some cases angioplasty, surgical thrombectomy, and thrombolysis.
- If the cause is venous thrombosis, the patient should be anticoagulated immediately (e.g., IV heparin), unless contraindicated.
- For AMI without evidence of vascular occlusion, the underlying condition should be treated; intra-arterial vasodilator infusion can be considered.
Key Points
- Consider AMI in elderly patients with a history of atrial fibrillation or vascular disease (even with a benign presentation and abdominal exam) or in younger patients with abdominal pain and a history of deep vein thrombosis (DVT) or hypercoagulable states.
- CTA is first-line imaging for diagnosis.
- Specific treatment varies based on etiology of AMI but includes prompt surgical consultation.
- Don’t delay in the diagnosis and management of AMI: time is not only tissue, but time is mortality!