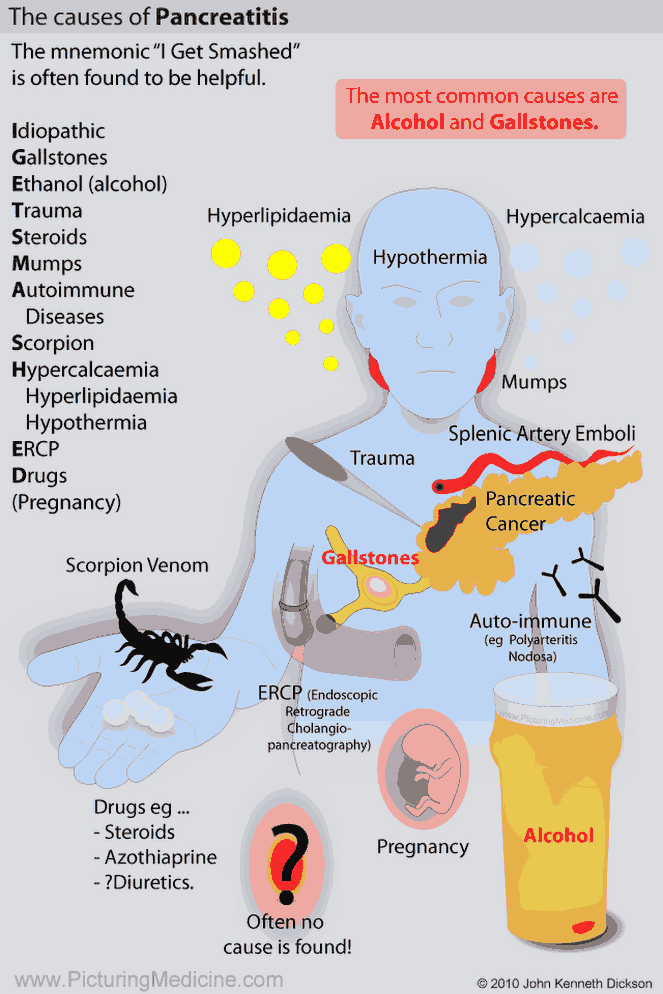
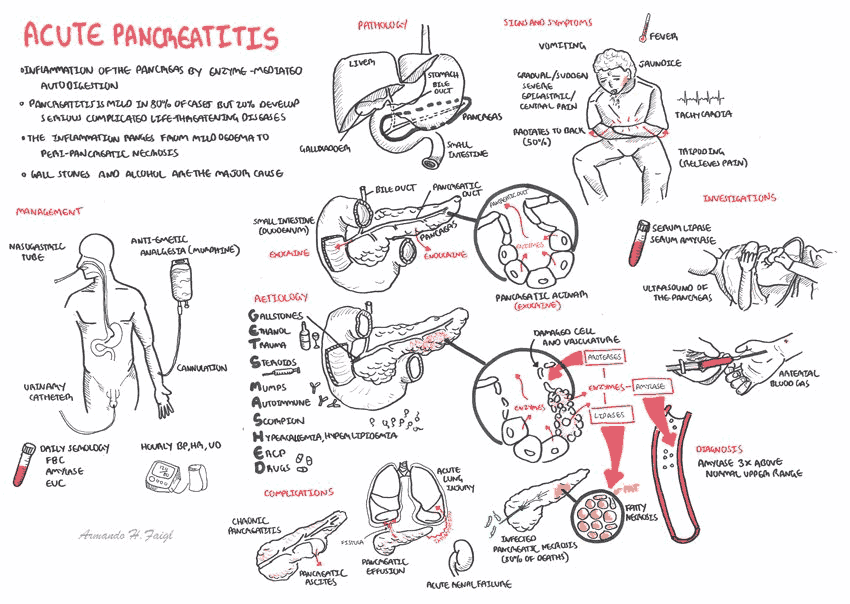
Etiology of Acute Pancreatitis
Causes of Acute Pancreatitis include:
- Gallstones (most cases)
- Alcohol (most cases)
- Idiopathic
- Hypercalcemia
- Hyperlipidemia
- Autoimmune
- Post ERCP
- Trauma
- Mumps
- Drugs (e.g., azathioprine,steroids or diuretics)
The causes of acute pancreatitis can be recalled from the mnemonic GET SMASH’D: gallstones, ethanol, trauma, steroids, mumps, autoimmune diseases, scorpion stings, hypertriglyceridemia, and drugs (e.g., azathioprine or diuretics).
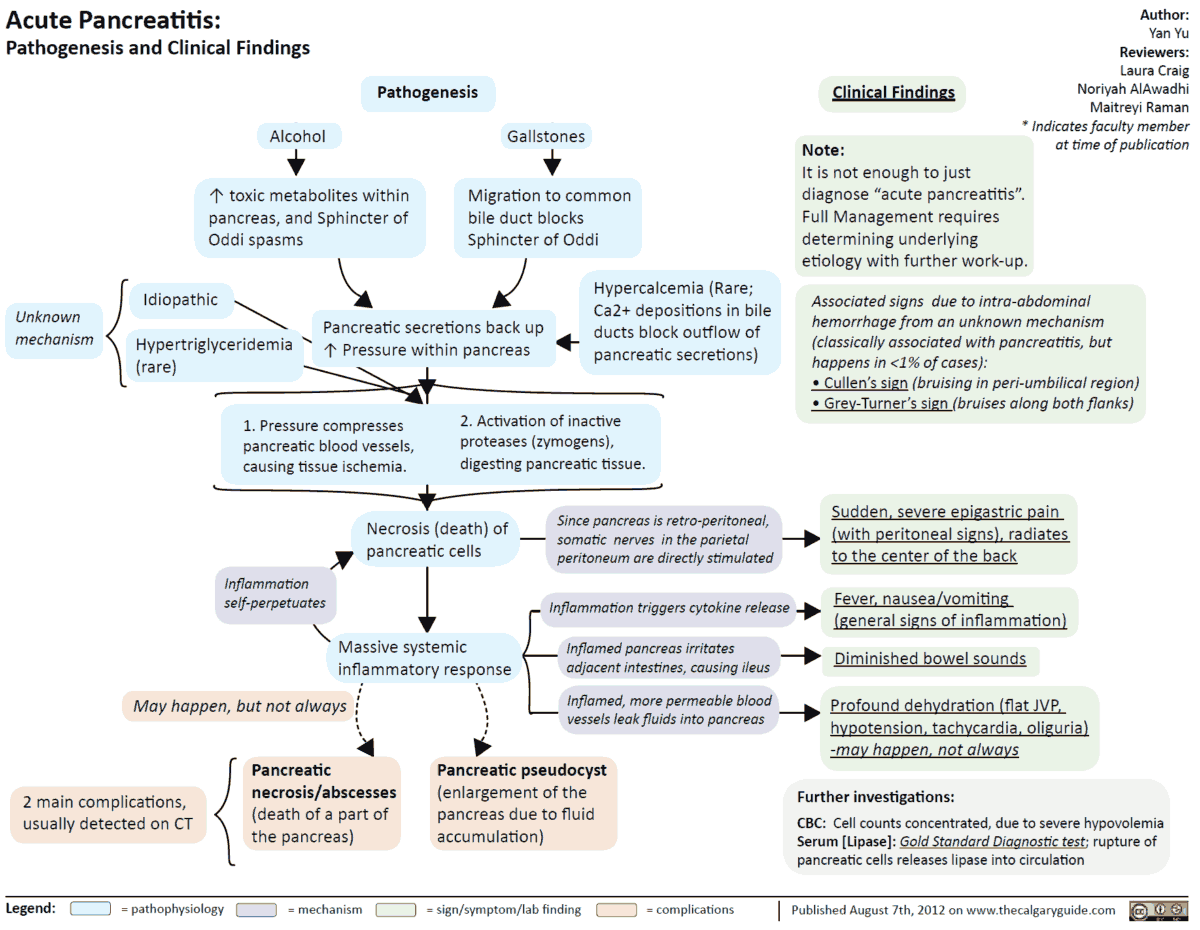
Clinical Features of Acute Pancreatitis
There may be a history of cholecystitis or other complications of gallstones. Alcohol intake should be ascertained.
The patient complains of:
- Severe abdominal pain radiating to the back or shoulder, which may be relieved by sitting forward
- There may be associated nausea and vomiting
On examination there is:
- abdominal tenderness with guarding and rebound tenderness
- tachycardia
- fever
- jaundice
- hypotension, and sweating
- bruising around the umbilicus (Cullen’s sign) or in the flanks (Grey-Turner’s sign)
Differential Diagnosis
- Any cause of an acute abdomen (e.g., cholecystitis, mesenteric ischemia, and intestinal perforation).
- Myocardial infarction
- Dissecting aortic aneurysm
Investigations
The following investigations are important in the patient with acute pancreatitis:
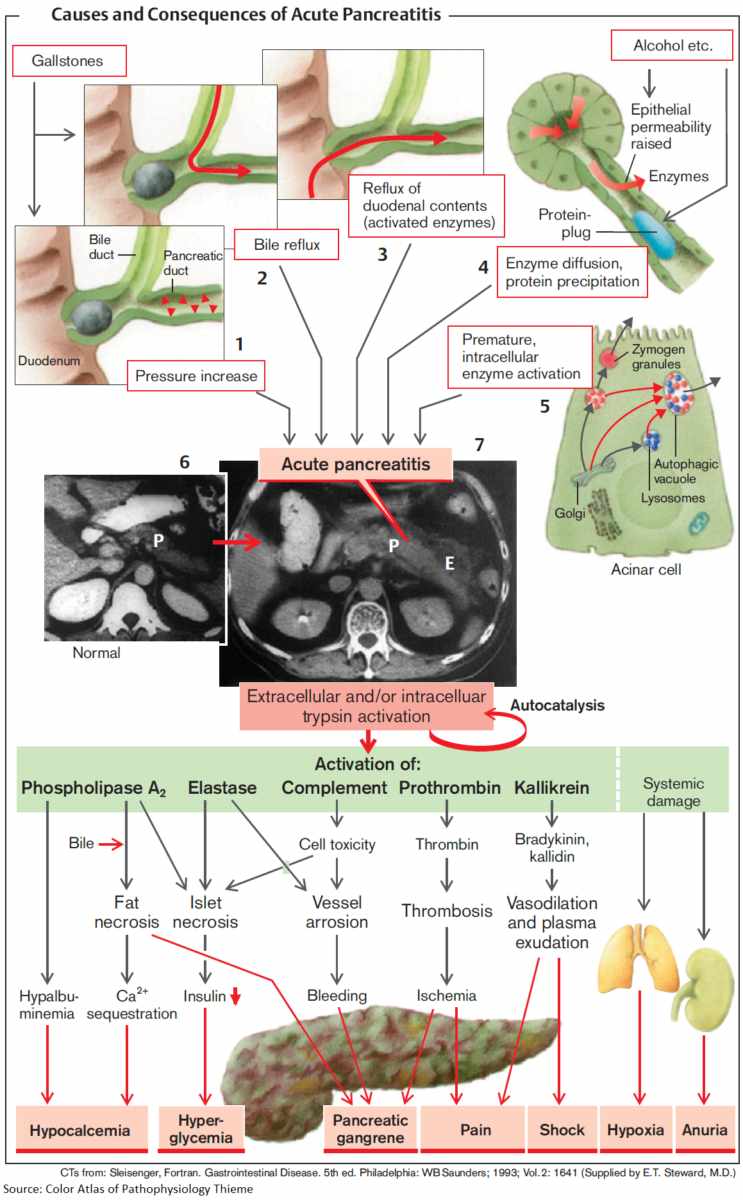
- Serum amylase: markedly raised (over 1000 IU/mL). Amylase is also raised with cholecystitis and perforated peptic ulcer, but usually to a lesser extent. Serum lipase is also elevated and is more specific than amylase.
- Abdominal x-ray: gallstones, pancreatic calcification indicating previous inflammation, an absent psoas shadow due to retroperitoneal fluid, and a distended loop of jejunum (“sentinel loop”).
- Serum calcium: may be low.
- White cell count: usually raised.
- ECG: to exclude myocardial infarction.
- Arterial blood gases: metabolic acidosis.
- CXR: widened mediastinum in aortic dissection; gas under the diaphragm in perforated peptic ulcer.
- Abdominal CT: assess severity.
READ MORE: Imaging of Acute Pancreatitis – to Image or Not to Image
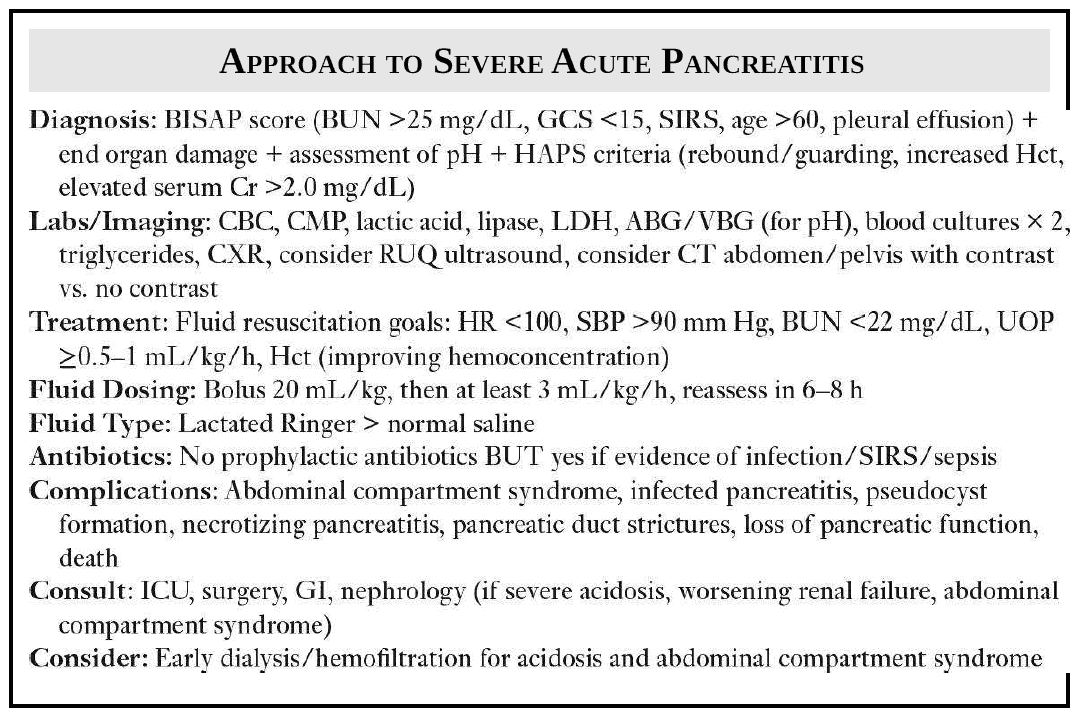
Management of Acute Pancreatitis
Management is usually conservative.
- Intravenous fluids should be given to maintain the circulating volume, and a central venous catheter may be helpful for assessing the volume of fluid required. If the patient is in shock (systolic blood pressure <90 mmHg), plasma expanders will be required.
- Pain relief is with intravenous or intramuscular opiates (e.g., pethidine, 50-150 mg 4 hourly, or pentazocine, 30-60 mg 4 hourly, meperidine, fentanyl, or morphine with an antiemetic such as prochlorperazine, 12.5 mg 8 hourly).
- A nasogastric tube should be inserted. TPN may be required.
- Blood tests, especially metabolic panel, glucose, and calcium, should be monitored.
- Surgery should be considered for suspected hemorrhagic necrosis of the pancreas.
- Some give H2-receptor antagonists, prophylactic antibiotics, or peritoneal lavage, although these measures are of unproven value.
READ MORE: Recognizing and Treating Severe Acute Pancreatitis (SAP)
Complications and Prognosis
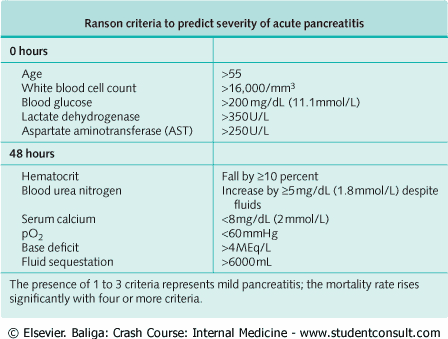
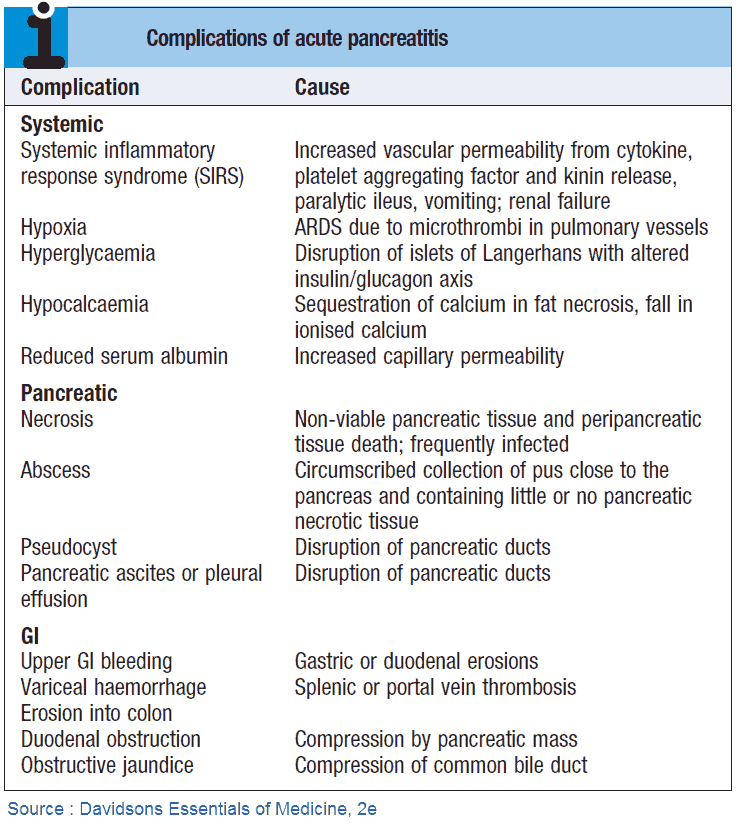
Ranson’s criteria are used to predict the severity of acute pancreatitis. Mortality is 5-10%, but recurrence is uncommon in patients who recover.
Complications include :
- shock
- renal failure
- sepsis
- respiratory failure
- hypocalcemia due to the formation of calcium soaps
- transient hyperglycemia
- pancreatic abscess requiring drainage
- pseudocyst (i.e., fluid in the lesser sac presenting as a palpable mass)
- persistently raised serum amylase or liver function tests, and fever
Patients should be investigated to exclude gallstones, and alcohol should be avoided.