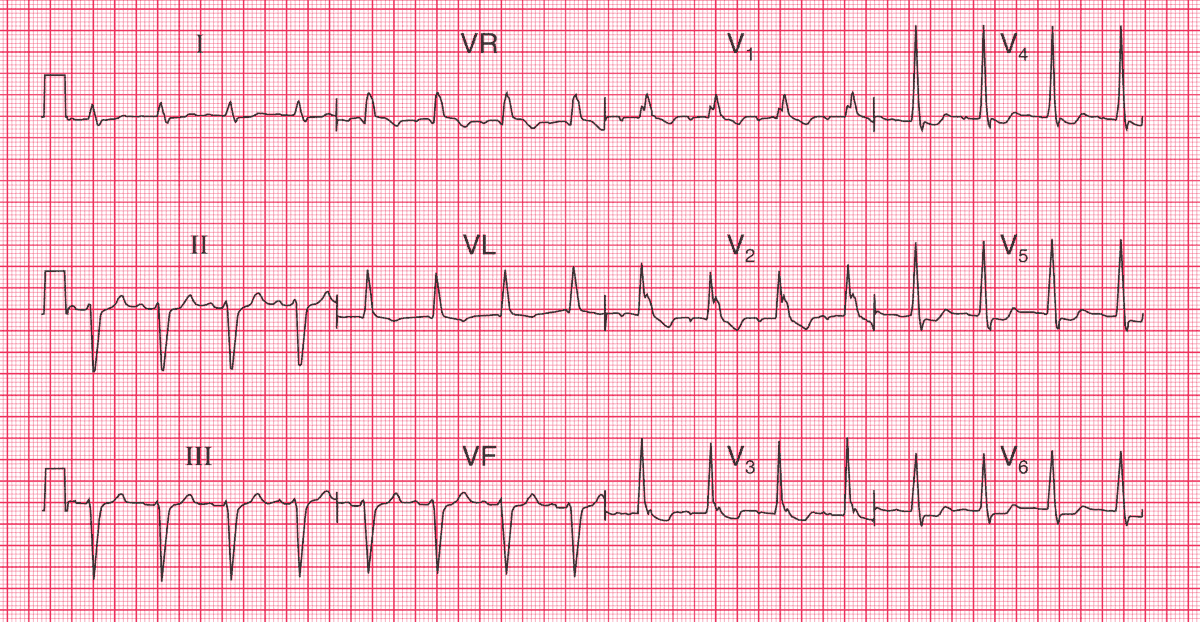
ECG Intepretation
- Sinus rhythm, rate 94/min
- PR interval at the upper limit of normal (200 ms)
- Left axis deviation
- QRS complex duration prolonged (160 ms)
- RSR1 pattern in leads V1–V2; wide S wave in lead V6
- Inverted T waves in leads VL, V1–V4
Clinical Interpretation
The left axis deviation is characteristic of left anterior hemiblock. There is also right bundle branch block (RBBB), so two of the main conducting pathways are blocked, resulting in ‘bifascicular block’.
The fact that the PR interval is at the upper limit of normal raises the possibility of delayed conduction in the remaining pathway; if the PR interval were definitely prolonged, this would indicate ‘trifascicular block’.
What to do ?
Bifascicular block is not an indication for pacing if the patient is asymptomatic. The problem here is to decide if the attacks of dizziness are due to intermittent complete heart block.
Ideally an ECG would be recorded during an attack – since they occur only every week or so, ambulatory ECG recording may not be helpful, but an event recorder would be worth trying.
In the absence of clear evidence, the decision whether or not to insert a permanent pacemaker is a matter of judgement, but in a patient with this story and ECG it would be a perfectly reasonable thing to do.
- READ MORE: ECG Interpretation: All you need to know
- More Similar Cases: RBBB and Left Posterior Fascicular Block (LPFB)