This article is an answer and interpretation to the ECG Case 156
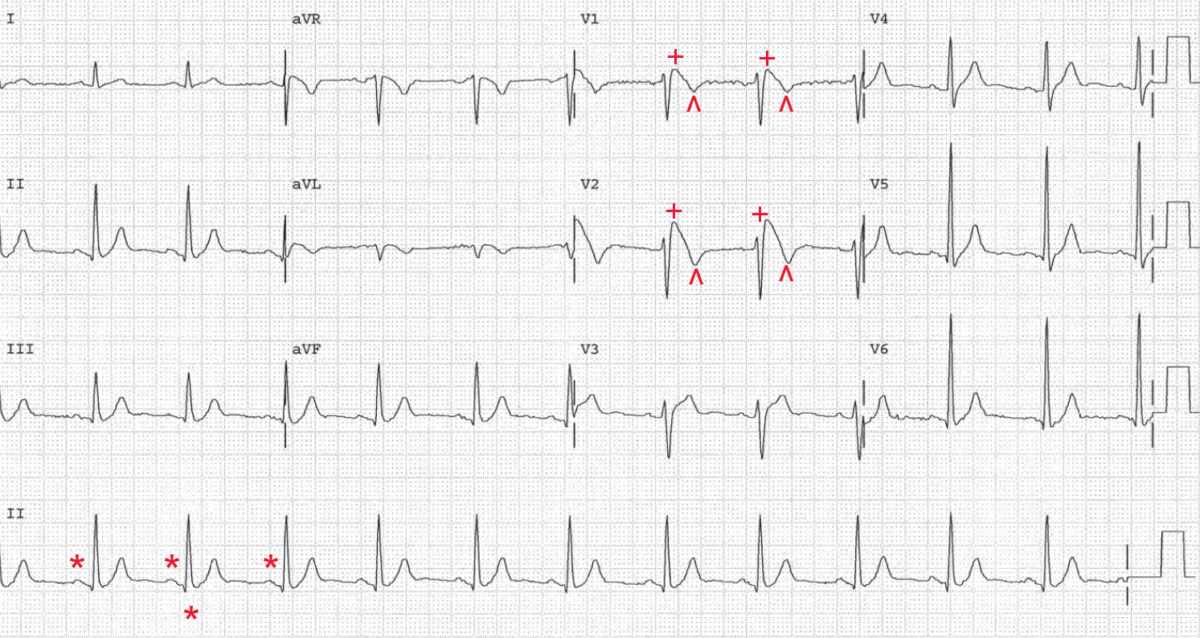
There is a regular rhythm at a rate of 72 bpm. There is a P wave (*) before each QRS complex, and the PR interval is stable (0.16 sec). The P wave is positive in leads I, II, aVF, and V4–V6 and negative in lead aVR. Hence this is a normal sinus rhythm.
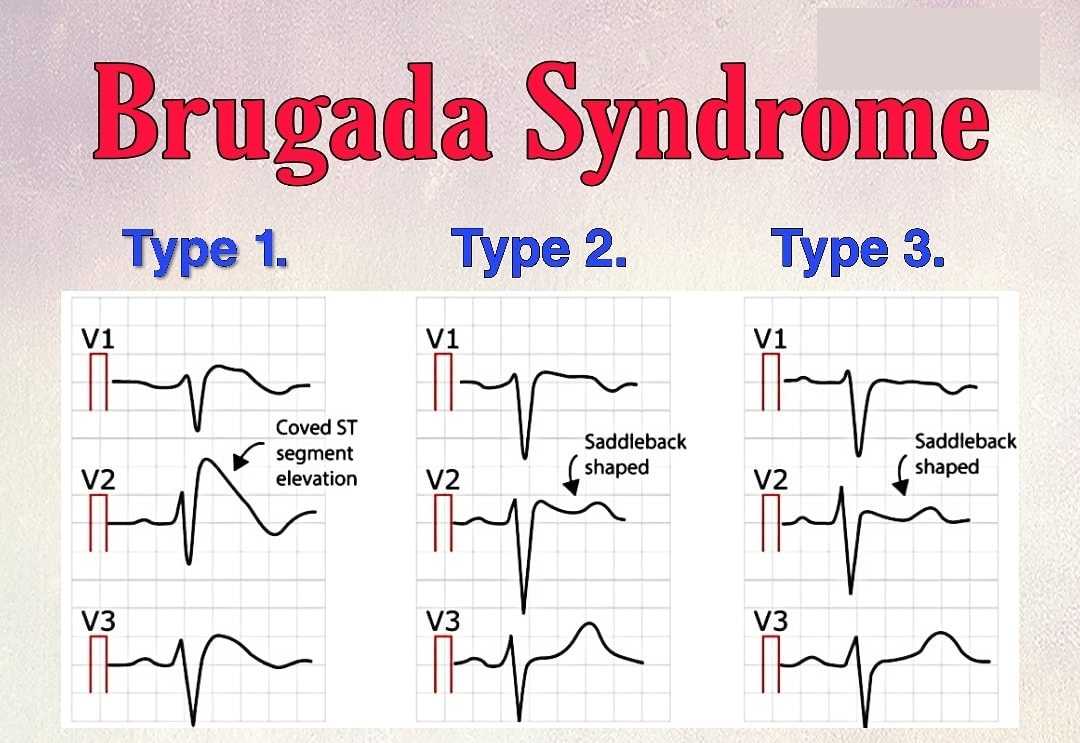
The QRS morphology is normal except in leads V1–V2. These leads show an elevated J point and ST segment (≥ 2 mm) (+) that descends slowly with an upward convexity to an inverted T wave (^). This has been termed a pseudo right bundle branch block (RBBB) pattern and is typical of a classic type 1 Brugada pattern.
The mechanism for the Brugada pattern is a genetic abnormality of the SCN5A sodium channel gene that affects sodium influx during the early part of phase 2 of the action potential. This alters the action potential of some, but not all of the ventricular myocardial cells.
The ventricular myocardium is composed of at least three electrophysiologically distinct cell types: epicardial, endocardial, and M cells. The ST-segment elevation and T-wave inversions seen in the right precordial leads in Brugada pattern are thought to be due to an alteration in the action potential in the epicardial and possibly the M cells, but not the endocardial cells.
The resulting dispersion of repolarization across the ventricular wall, which is most pronounced in the right ventricle, results in a transmural voltage gradient that is manifested in the ECG as J-point and ST-segment elevation.
Patients with arrhythmia associated with the Brugada pattern have the Brugada syndrome. All clinical manifestations of the Brugada syndrome are related to life-threatening ventricular arrhythmias (often manifest as syncope or sudden cardiac arrest).
Sudden cardiac arrest may be the first and only clinical event in the Brugada syndrome. Although pharmacologic therapy, particularly quinidine, may be of some benefit, the therapy of choice for patients with symptoms is an implantable cardioverter-defibrillator (ICD).