Emergency providers (EPs) interpret electrocardiograms (ECGs) on a daily basis for a variety of clinical scenarios. An ECG is most commonly obtained for the emergency department (ED) patient with acute chest pain.
In these patients, it is imperative to diagnose an ST-segment elevation myocardial infarction (STEMI), as emergent reperfusion therapy is indicated.
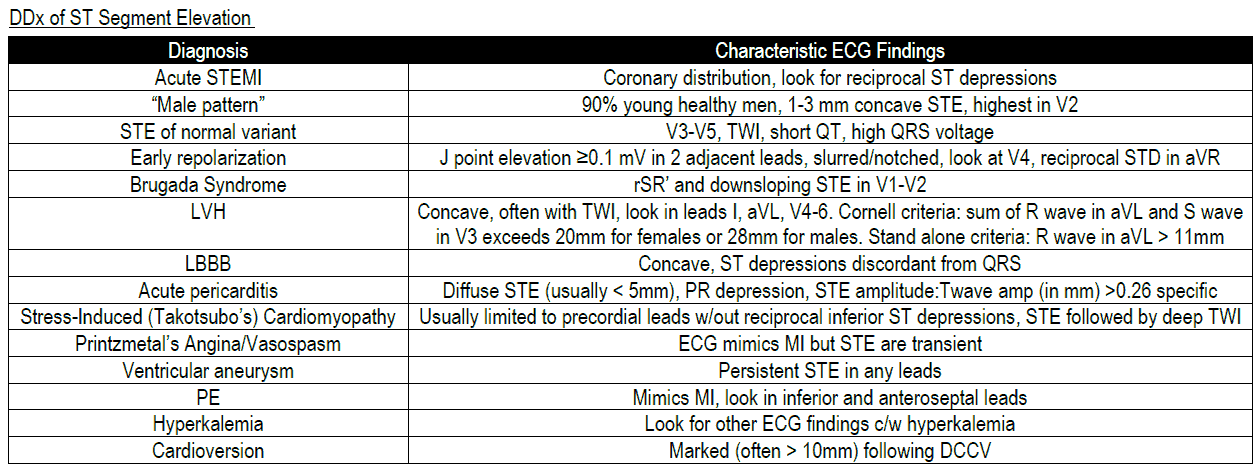
Notwithstanding, there are numerous conditions that cause ST-segment elevation (STE) on an ECG that are not attributable to an acute coronary syndrome. In order to avoid errors in diagnosis or management, it is important for the EP to know the differential diagnosis for STE.
Nonischemic causes of ST Elevation include:
- Normal Variant ST Elevation
- Early Repolarization
- Brugada Syndrome
- LVH
- LBBB
- Acute Pericarditis
- Left ventricular aneurysm
- Stress Induced (Takotsubo) Cardiomyopathy
- Printzmetal Angina / Vasospasm
- Pulmonary Embolism
- Hyperkalemia
- Post Cardioversion
Early Repolarization
Early repolarization is a common cause of ST Elevation. It is typically seen in males younger than 45 years of age and in athletic patients. Recent literature has demonstrated that early repolarization is a risk factor for sudden cardiac death, as it increases the risk for idiopathic ventricular fibrillation.
Early repolarization typically produces a notched J-point with STE that is <3 mm on the ECG.
There is currently no specific treatment for early repolarization. Patients should be instructed to follow up with their primary care physician.
Cardiology referral is appropriate for patients who have a personal or family history of sudden cardiac death or additional ECG findings that suggest the presence of coronary artery disease.
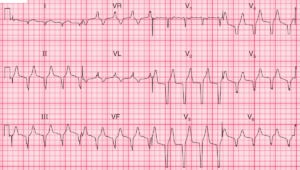
Pericarditis
Pericarditis is another condition that should be considered in the differential diagnosis of STE. Patients typically present with acute chest pain that is sharp, pleuritic and positional, exacerbated by inspiration and relieved by sitting forwards. A friction rub on auscultation is pathognomonic of pericarditis.
ECG features of pericarditis that help to distinguish it from STEMI are :
- The ST segment elevation is typically widespread, affecting all of those leads (anterolateral and inferior) that ‘look at’ the inflamed epicardium. Leads aVR and V1 usually show reciprocal ST segment depression.
- The ST segment elevation is characteristically ‘saddle shaped’ (concave upward).
- T wave inversion occurs only after the ST segments have returned to baseline.
- Q waves do not develop.
- Depression of the PR segment that may be seen in any leads except aVR and V1 (where there may be PR segment elevation)
- The ECG changes seen in pericarditis typically occur over the course of several weeks, in contrast to rapid evolution of ST segment changes seen in STEMI
PR-segment depression is commonly thought to be pathognomonic for pericarditis; however, this finding can be transient and can also be seen in patients with an STEMI.
ECG features that favor STEMI over Pericarditis:
- Reciprocal ST-segment depression or T-wave inversions
- ST Elevation that is flat or horizontal should be considered an STEMI until proven otherwise.
- Rapid evolution of ST segment changes during the course of the ED evaluation is more suggestive of an acute coronary syndrome in contrast to pericarditis.
Left bundle-branch block (LBBB)
In the setting of LBBB, the ST segment is directly opposite to that of the main QRS complex vector. In leads V1 to V3, the QRS vector is negative, thereby producing ST Elevation.
This discordant STE is typically less than 5 mm in the setting of LBBB. Patients with a pacemaker will also demonstrate STE similar to a LBBB.
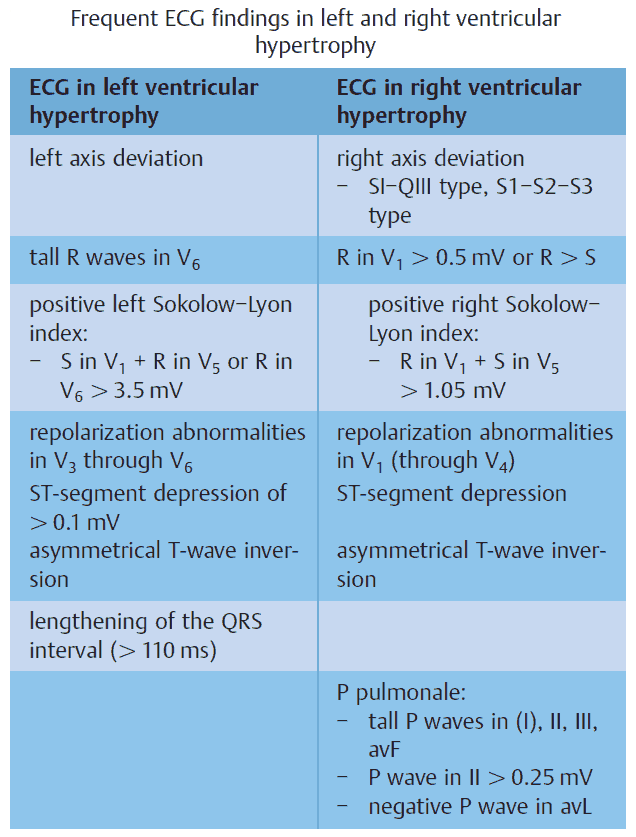
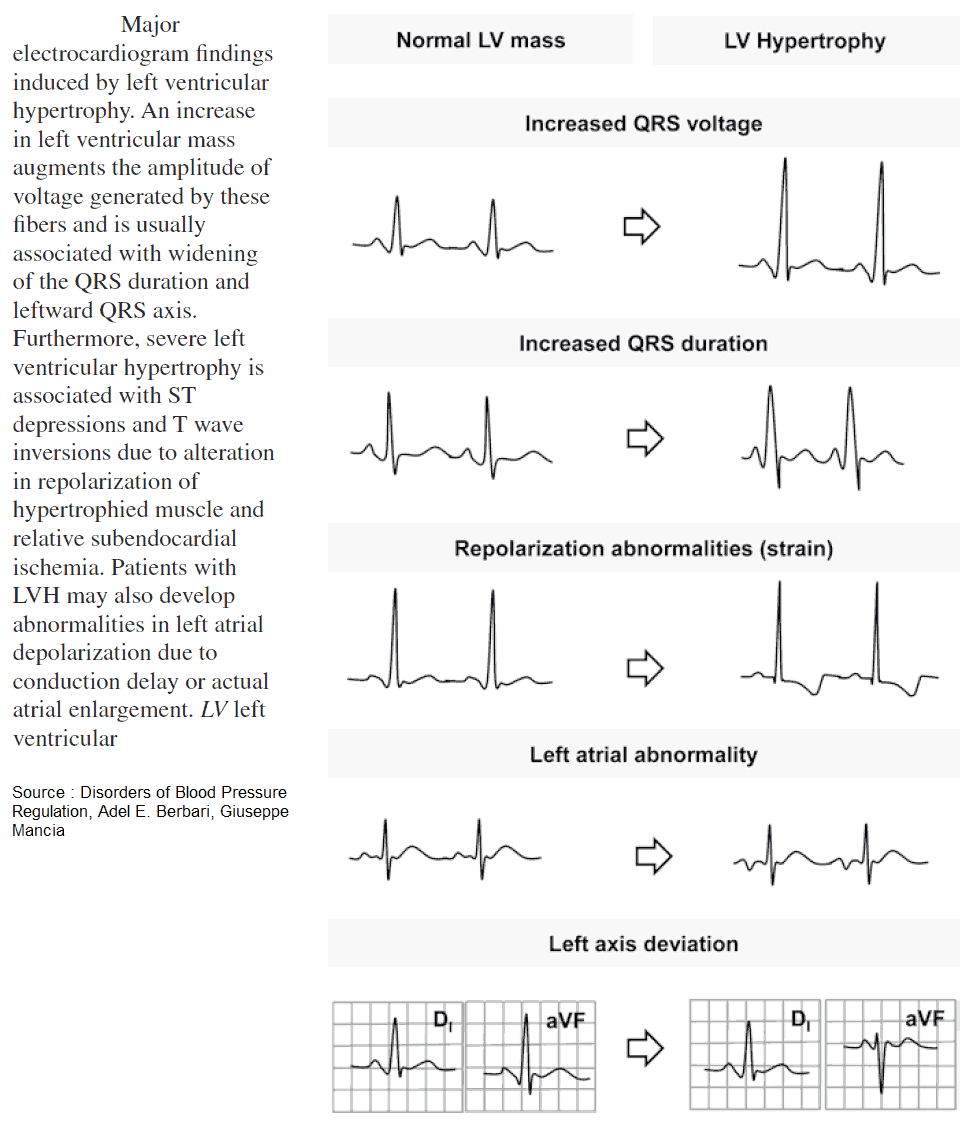
Left Ventricular Hypertrophy (LVH)
LVH produces discordant ST Elevation, with a deep S wave in leads V1 to V3 and a tall R wave in leads I, aVL, V5, and V6.
Left Ventricular Aneurysm
Patients with a left ventricular aneurysm may have STE along with deep anterior or septal Q waves in leads V1 to V3.
Similar to pericarditis, LBBB, LVH, and left ventricular aneurysm do not cause dynamic ECG abnormalities.
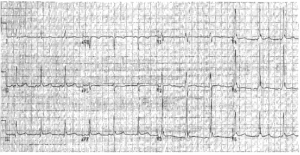
Hyperkalemia
Hyperkalemia is often referred to as the “great imitator” of ECG abnormalities. Hyperkalemia can produce numerous ECG findings that can easily be misdiagnosed and incorrectly treated.
It is well known to cause the appearance of ST Elevation, as the T-wave is pulled to a peak. Additional signs of hyperkalemia include peaked T-waves, bradydysrhythmias, tachydysrhythmias, and widened QRS complexes.
Prinzmetal Angina and Takotsubo Cardiomyopathy
Less common causes of ST Elevation include Prinzmetal angina and takotsubo cardiomyopathy. Both of these clinical entities are often diagnosed as STEMI in patients with acute chest pain. These diagnoses are often made following emergent cardiac catheterization.
Key Points
- STEMI is not the only cause of STE.
- Dynamic ECG abnormalities are more consistent with an acute coronary syndrome.
- Nonischemic causes of STE include early repolarization, LBBB, LVH, pericarditis, and left ventricular aneurysm.
- Hyperkalemia should be considered in the differential diagnosis of STE.
- The diagnosis of Prinzmetal angina or takotsubo cardiomyopathy is often made following emergent cardiac catheterization for presumed STEMI.
Suggested Readings
- Hanna EB, Glancy DL. ST-segment elevation: Differential diagnosis caveats. Cleve Clin J Med. 2015;82(6):373–384.
- Huang HD, Birnbaum Y. ST elevation: Differentiation between ST elevation myocardial infarction and nonischemic ST elevation. J Electrocardiol. 2011;44(5):494.e1–494.e12.
- Toledano K, Rozin AP. Early repolarization: Innocent or dangerous? Am J Med Sci. 2013; 346(3):226–232.