Pediatric cancer presents unique diagnostic and therapeutic challenges due to its non-specific symptoms and rapid progression.
Each year, an estimated 400,000 children and adolescents (0–19 years) are diagnosed with cancer worldwide, according to the World Health Organization. Common pediatric cancers include blood cancers, brain malignancies, lymphatic cancers, and solid tumors like Wilms’ tumor and neuroblastoma. While survival rates exceed 80% in high-income countries, they remain below 30% in low- and middle-income countries (LMICs).
In this article, we’ll discuss:
- Key diagnostic strategies used in pediatric oncology
- Current therapeutic approaches for treating childhood cancers
- Methods to enhance early detection of pediatric malignancies
- Factors contributing to global disparities in treatment outcomes
- Evidence-based practices aimed at improving prognosis and care quality
Clinical Presentation and Diagnostic Barriers
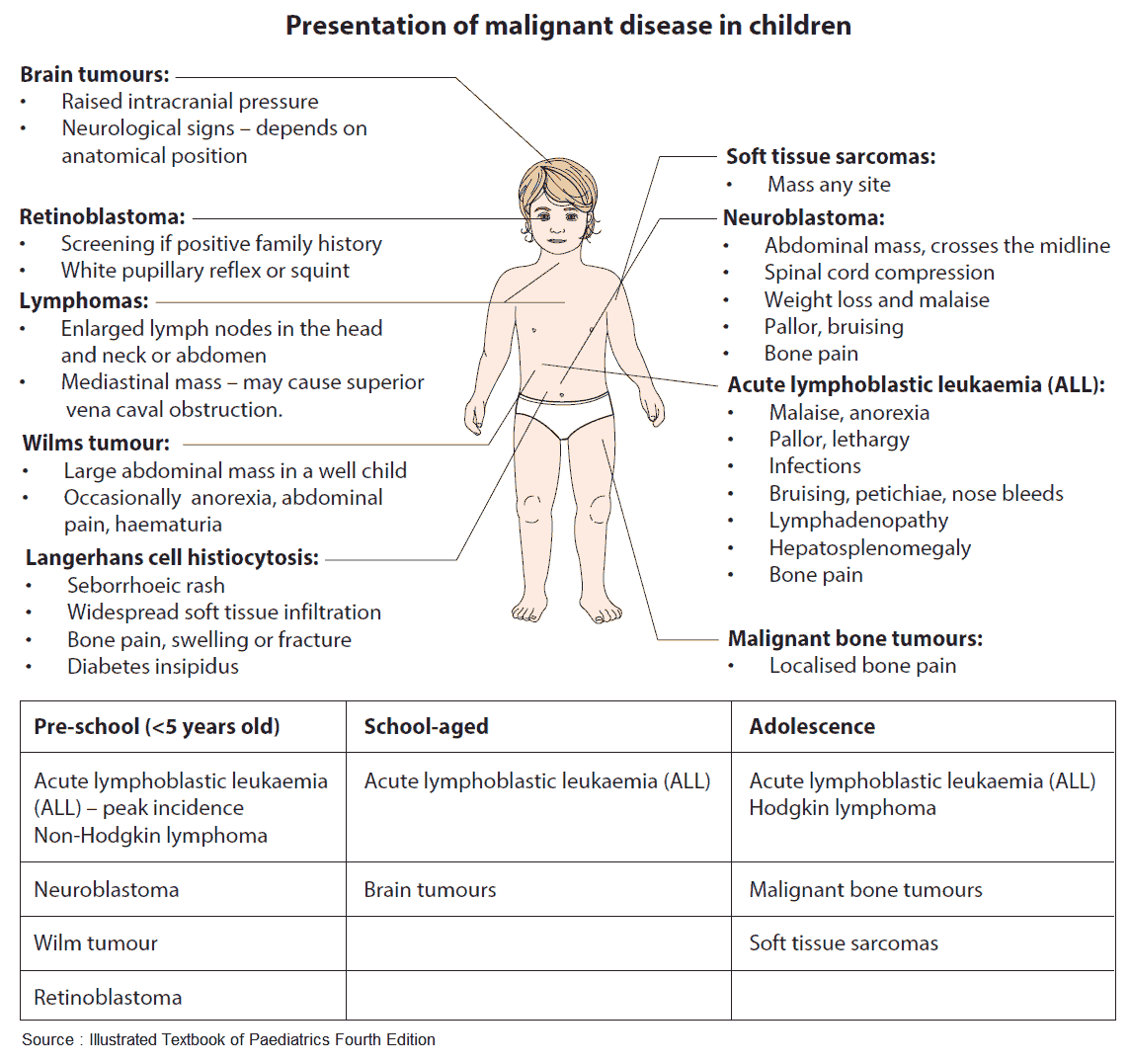
Pediatric cancers often present with vague, non-specific symptoms such as fatigue, pallor, persistent pain, or recurrent infections, frequently mistaken for common childhood illnesses. This overlap can lead to delayed clinical suspicion and misdiagnosis, especially in primary care settings.
A study published in ScienceDirect highlights the complex barriers affecting timely access to pediatric oncology services. These barriers operate at systemic, societal, and individual levels, contributing to diagnostic delays and suboptimal outcomes. In particular, the study emphasizes the impact of:
- Systemic limitations, such as workforce shortages and uneven distribution of diagnostic resources.
- Financial toxicity, leading to delayed care-seeking or treatment discontinuation.
- Socioeconomic and racial disparities exist, where marginalized populations experience longer diagnostic intervals and limited access to specialized care.
Diagnostic Modalities in Pediatric Oncology
Accurate diagnosis and staging in pediatric oncology rely on a combination of imaging techniques, each with specific strengths and limitations.
Radiography
Radiography remains a common starting point, accounting for about 66% of all imaging exams in children in the U.S.
- Useful for detecting:
- Mediastinal adenopathy in lymphoma
- Skeletal tumors such as Ewing sarcoma or osteosarcoma
- Typically followed by more advanced imaging for confirmation and staging
Ultrasound
It is widely accessible and preferred for evaluating superficial structures.
- Often sufficient for:
- Thyroid malignancies
- Testicular tumors
- Limitations include:
- Inability to visualize deep or aerated regions (e.g., lungs)
Computed Tomography (CT)
CT scans are critical for staging, especially in thoracic and abdominopelvic tumors.
- Advantages:
- Rapid image acquisition
- High resolution, especially with IV iodine-based contrast
Magnetic Resonance Imaging (MRI)
MRI provides excellent soft tissue contrast and avoids ionizing radiation.
- Best suited for:
- Central nervous system and soft tissue tumors
- Limitations:
- Longer scan times, higher cost, and limited lung imaging capability
Nuclear Medicine (NM)
NM offers functional imaging to assess tumor metabolism and spread.
- Commonly used in:
- Neuroblastoma
- Lymphoma
- Bone metastases
Together, these modalities support precise diagnosis, guide treatment planning, and monitor therapeutic response in pediatric oncology care.
Therapeutic Approaches in Pediatric Cancers
Pediatric cancer treatment relies on a multimodal approach tailored to the specific diagnosis, stage, and patient condition. Therapeutic strategies aim to maximize cure rates while minimizing long-term adverse effects. According to the American Cancer Society, the primary treatment modalities include:
Surgery
It is used to remove tumors, collect biopsy samples, or place devices like central lines or feeding tubes. It is often the first step in managing solid tumors and may be combined with other therapies for better outcomes.
Radiation Therapy
It uses high-energy beams to destroy cancer cells and is commonly used before or after surgery or chemotherapy. The treatment itself is painless, but side effects depend on the dosage and the area being treated.
Chemotherapy
It involves the use of cytotoxic and targeted drugs to kill or inhibit cancer cells. These drugs are given by IV, orally, injection, or into the spinal fluid, based on cancer type and treatment plan.
Stem Cell Transplantation
It is also known as a bone marrow transplant. This therapy allows for high-dose chemotherapy by restoring the bone marrow with healthy stem cells. It is typically used in aggressive or relapsed cancers where intensive treatment is required.
Role of Advanced Practice Providers in Pediatric Oncology Care
Advanced practice providers (APPs), including nurse practitioners and physician assistants, play an essential role in pediatric oncology by supporting diagnosis, treatment, and long-term care. Their responsibilities range from symptom management and medication monitoring to coordinating multidisciplinary care and educating families.
Providers trained through specialized pathways, such as the MSN-FNP program, are equipped with advanced clinical skills. Their pediatric-focused knowledge enables them to deliver comprehensive care in both hospital and outpatient settings.
Cleveland State University states that these practitioners help bridge gaps in access and improve continuity of care. It prepares them to deliver both primary and specialty care. Graduates are trained to serve patients of all ages across diverse healthcare settings.
Challenges in Low-Resource and Rural Settings
Pediatric oncology care in low-resource and rural settings faces significant obstacles that impact early diagnosis, timely treatment, and overall survival. Limited access to specialized healthcare providers, diagnostic equipment, and oncology medications often leads to delays in care.
Geographic barriers, lack of referral systems, and financial constraints further compound these challenges. In many cases, children present with advanced-stage disease due to missed early signs and poor follow-up. Improving outcomes in underserved regions requires stronger infrastructure, better telemedicine access, and targeted provider training.
Future Directions and Research Opportunities
Advancements in pediatric oncology continue to focus on therapies that offer greater precision and reduced long-term toxicity. According to the National Cancer Institute (NCI), two major areas of ongoing research include:
Immunotherapy
Immunotherapies like CAR T-cell therapy have shown success in treating certain childhood leukemias, particularly acute lymphoblastic leukemia. Clinical trials led by the NCI Pediatric Oncology Branch are evaluating immunotherapy approaches across various pediatric cancers. Additional studies are being conducted by the Children’s Oncology Group (COG) and the Pediatric Brain Tumor Consortium (PBTC).
Molecularly Targeted Therapy
These therapies work by disrupting specific molecular pathways critical to cancer cell growth. One example is selumetinib, a targeted agent that has demonstrated tumor reduction in children with low-grade gliomas. It is currently under investigation in phase 3 trials supported by COG and PBTC.
These efforts support the National Cancer Plan’s goal of providing safer, more effective treatments for pediatric patients.
Frequently Asked Questions
Which tests help confirm the diagnosis?
Diagnostic confirmation in pediatric cancer typically involves a combination of imaging studies such as MRI, CT, or ultrasound. It also includes blood tests and a biopsy of the suspected tumor. These tests help identify the cancer type, stage, and guide appropriate treatment planning.
In what ways do childhood cancers differ from those seen in adults?
Pediatric cancers differ from adult cancers in type, biology, and response to treatment. They often involve rapidly growing cells, like in leukemia or brain tumors. Unlike many adult cancers, pediatric cancers are less linked to lifestyle factors and generally respond better to intensive therapies.
What trends are shaping pediatric oncology?
Pediatric oncology is being shaped by advances in immunotherapy and molecularly targeted treatments, offering more personalized and less toxic options. CAR T-cell therapy and targeted drugs are improving outcomes and advancing precision medicine in childhood cancer care.
Advancing Equity and Innovation in Pediatric Cancer Care
Timely diagnosis and personalized treatment remain central to improving outcomes in pediatric oncology. With advancements in imaging, targeted therapies, and immunotherapy, the landscape of childhood cancer care is evolving rapidly.
However, disparities in access, especially in low-resource settings, continue to challenge progress. Strengthening healthcare infrastructure, expanding specialized training, and supporting ongoing research are essential to ensuring all children receive early and effective cancer care.
This article is a guest contribution submitted by a professional healthcare writer and reviewed for accuracy.