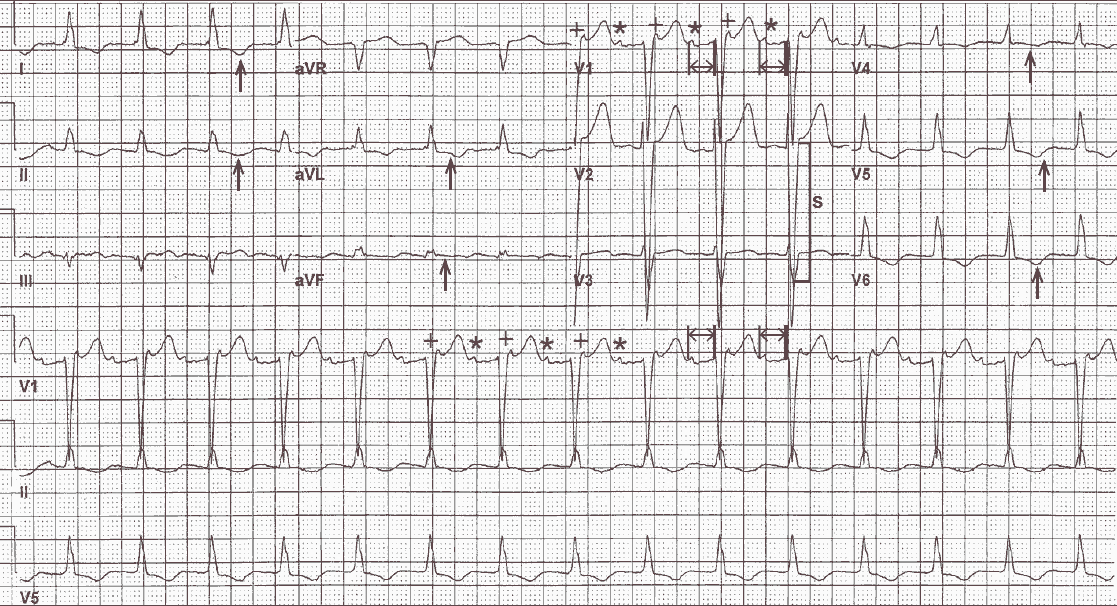
The rhythm is regular at a rate of 90 bpm. Evidence of atrial activity can be seen, primarily in lead V1 (*). The atrial rate is regular and the PR interval (↔) is constant (0.28 sec).
Although this appears to be a sinus rhythm with a first-degree AV block, there is an abnormality noted at the end of the QRS complex in lead V1 (+), which looks like an R′ waveform but has a morphology similar to the obvious P wave.
In addition, the interval between the P waves and this waveform at the end of the QRS complex is regular, at a rate of 180 bpm. Although atrial activity is not seen in the other leads, the most likely diagnosis is atrial tachycardia with 2:1 AV block.
The QRS complex duration is prolonged (0.12 sec) with pattern of LBBB. The amplitude of the QRS complex is increased, particularly the S wave in lead V2 (30 mm [ ] ] ), which satisfies one of the criteria for left ventricular hypertrophy (LVH, ie, S-wave depth or R-wave amplitude in any precordial lead ≥ 25 mm). There are ST-T wave changes (↑) in leads I, aVL, aVF, and V3-V6, possibly associated with LBBB and LVH.
Atrial Tachycardia
Atrial tachycardia is not a common arrhythmia and may be associated with digoxin toxicity, especially when there is AV block (ie, atrial tachycardia with block). Digoxin also causes an increase in peripheral vagal tone that slows and blocks conduction through the AV node. A digoxin level should be obtained and digoxin withheld.
However, other causes of atrial tachycardia include:
- cardiomyopathy with heart failure
- pulmonary disease
- myocardial infarction
- alcohol excess
- hypokalemia
- hypoxia
- sympathomimetic agents
- cocaine.
In these situations AV block may be the result of underlying AV nodal disease.