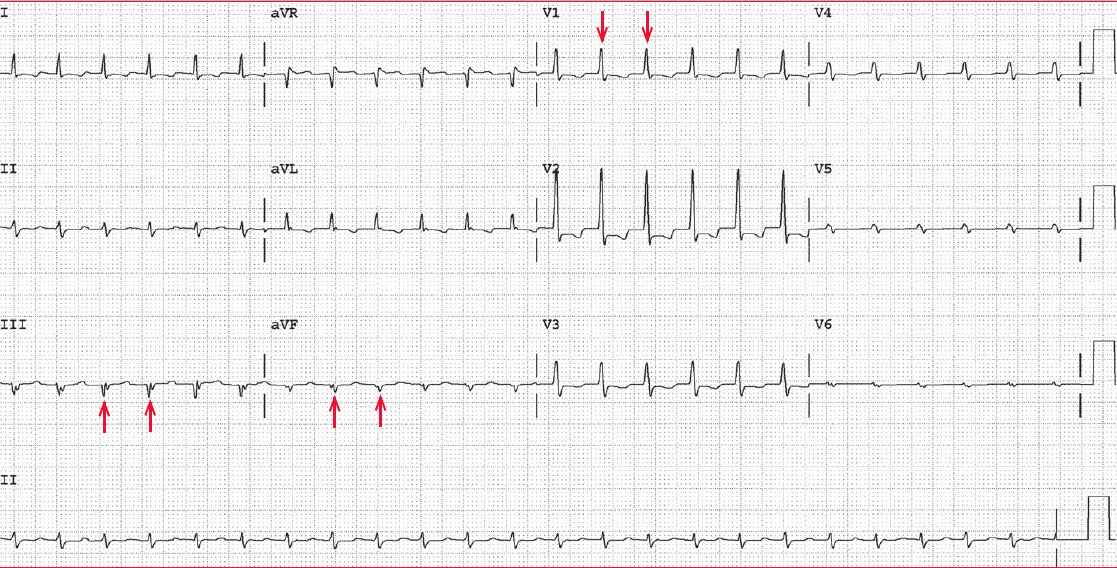
The ECG shows a regular rhythm at a rate of 140 bpm. The QRS complex duration is normal (0.08 sec), as are the QT/QTc intervals (280/430 msec).
The axis is leftward (positive QRS complex in leads I and II and negative QRS complex in lead aVF), but the negative QRS complex in lead aVF is the result of a Q wave (↑). There is also a Q wave in lead III (↑↑). Q waves in leads II and III are diagnostic for an inferior wall myocardial infarction.
In addition, there is a tall R wave in lead V1 (↓) (R/S ratio > 1 or R-wave amplitude > 7 mm); along with an inferior wall myocardial infarction, this is most likely the result of posterior wall involvement. However, other causes for a tall R wave in lead V1 include the following:
- Right ventricular hypertrophy (usually associated with a right axis and right atrial hypertrophy)
- Wolff-Parkinson-White pattern (short PR interval and widened QRS complex due to a delta wave)
- Hypertrophic cardiomyopathy (septal hypertrophy with prominent septal Q waves) and usually left ventricular hypertrophy
- Early transition (counterclockwise rotation)
- Duchenne muscular dystrophy (associated with a posterolateral infarct pattern)
- Dextrocardia (reverse R-wave progression in leads V1-V6, right axis, negative P and T waves in leads I and aVL and positive P and T waves in lead aVR)
- Lead switch (leads V1, V2, V3)
- Right-sided leads with reverse R-wave progression
- Normal variant
Also noted are ST-segment depressions, especially in lead V2, along with T-wave abnormalities. These findings are consistent with posterior wall involvement.
There are no P waves before or after the QRS complexes. Hence this is no-RP junctional tachycardia. The most common etiology for this is atrioventricular nodal reentrant tachycardia (AVNRT).