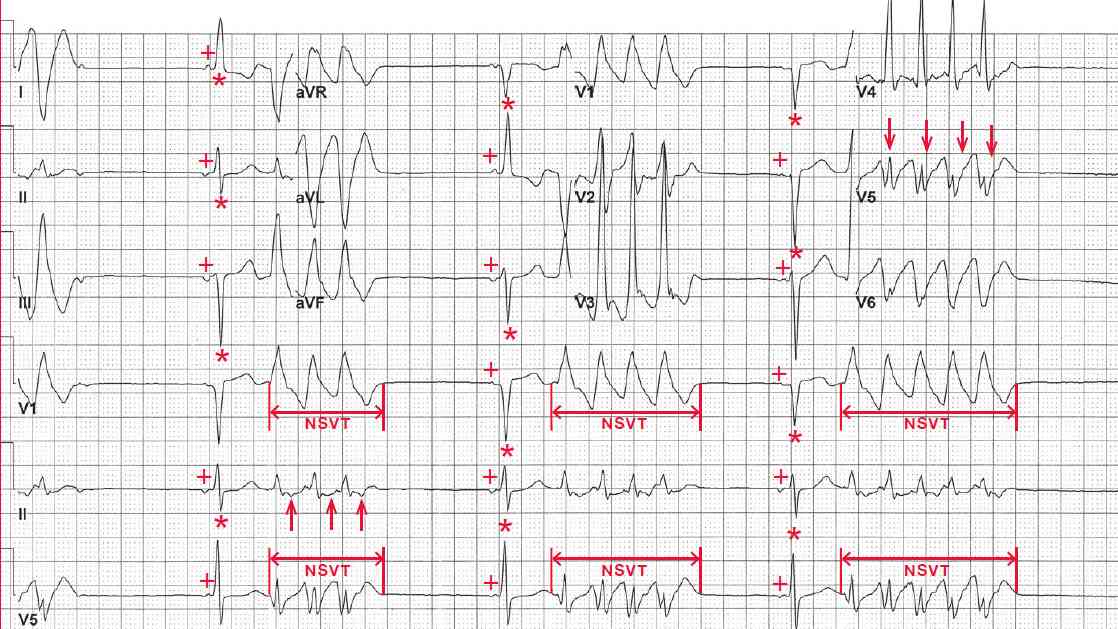
There are three narrow QRS complexes (0.10 sec) (*) that are preceded by a P wave (+) with a constant PR interval (0.14 sec). However, the P waves are negative in leads II and aVF and negative–positive in lead V5. They are, therefore, not sinus in origin but rather ectopic atrial beats. They have a left axis, between 0° and –30° (positive QRS complex in leads I and II and negative QRS complex in lead aVF).
After each narrow QRS complex there are episodes of three to five QRS complexes (↔), at a rate of 200 bpm. The QRS complexes are wide (0.16 sec) with an abnormal morphology. Although they have the same basic morphology, subtle differences can be seen in the QRS complexes (↓) and ST-T waves (↑).
Therefore, the wide QRS complexes are ventricular and this is monomorphic nonsustained ventricular tachycardia, defined as more than three sequential QRS complexes lasting up to 30 seconds. Wide complex tachycardias are due to either ventricular tachycardia or supraventricular tachycardia with aberrancy (ie, raterelated or underlying bundle branch block).
Other features in addition to the variability of QRS complex and ST-T wave morphology that point toward a ventricular origin for this wide complex tachycardia include a QRS complex width of 160 msec or greater and a QRS complex morphology that is not consistent with either a left (LBBB) or right (RBBB) bundle branch block, particularly the lack of an RSR′ pattern in lead V1 and an R-wave amplitude that is less than the S-wave depth in lead V6.
Alternatively, an RSR′ pattern in lead V1 and an R-wave amplitude that is taller than the S-wave depth in lead V6 are the typical findings of supraventricular tachycardia with RBBB. In addition, there is an R/ S complex in lead V2 and the R wave (> 100 msec) is wider than the S wave and it is greater than 100 msec in duration. This is consistent with a ventricular origin.
The R wave that is wider than the S wave indicates that initial ventricular activation is abnormal, ie, a ventricular complex. With a rate-related aberration the initial forces of the QRS complex are normal (ie, the R-wave width is less than 100 msec and narrower than the S-wave amplitude), whereas with a ventricular complex the initial forces are slow as a result of activation that is not via the normal Purkinje fibers but rather directly through the ventricular myocardium.
The anatomic origin of ventricular tachycardia can be determined from a 12-lead ECG. If the R-wave amplitude is taller than the S-wave depth in lead V1 (R>S), then the tachycardia has an RBBB-like morphology and, therefore, most likely originates in the left ventricle.
Leads in which the QRS complex is primarily negative in deflection represent the origin of the tachycardia (ie, the electrical vector is moving away from the origin and hence these leads). In this case, the QRS complex is negative in leads I and aVL; therefore, the ventricular tachycardia originates from the lateral wall of the left ventricle. The tachycardia is positive in leads II, III, and aVF and hence is inferiorly directed.