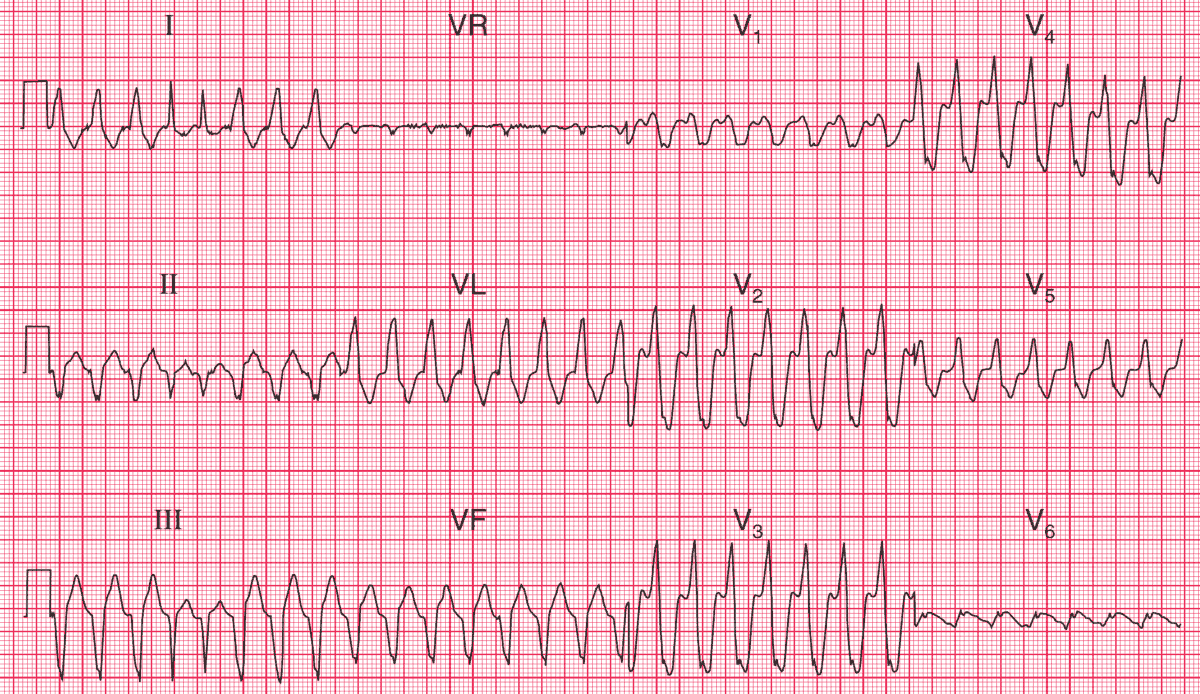
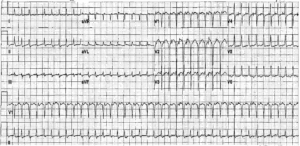
ECG Interpretation
- Broad complex tachycardia at about 188/min
- No P waves visible
- Left axis deviation
- QRS complex duration about 140 ms
- Narrow fourth and fifth QRS complexes
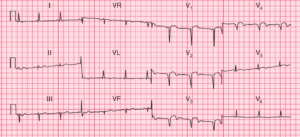
Clinical Interpretation
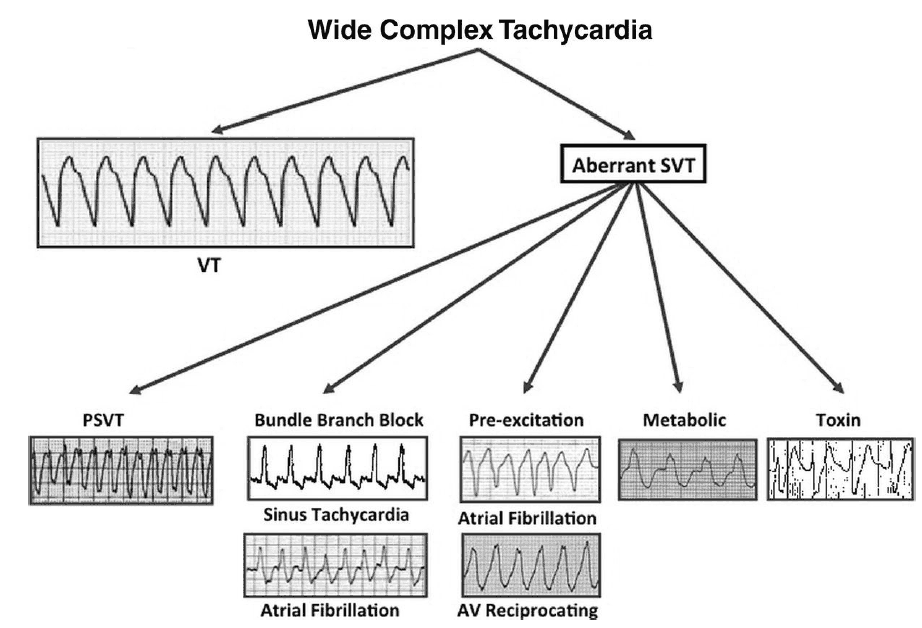
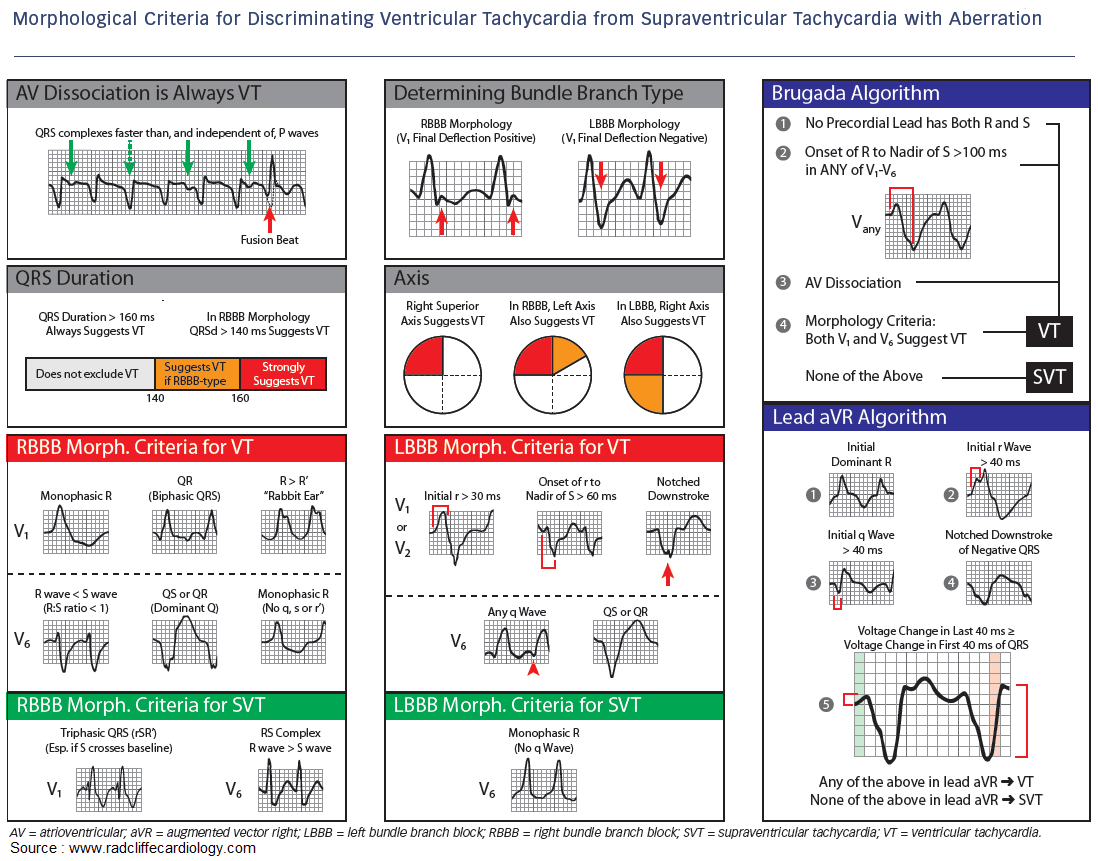
Broad complex tachycardias may be ventricular, supraventricular with bundle branch block, or due to the Wolff–Parkinson–White syndrome.
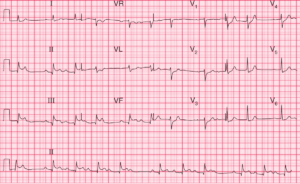
We have no ECG from this patient recorded in sinus rhythm, which is always the most helpful thing in deciding between these possibilities.
The complexes are not very wide, which would be consistent with a supraventricular origin with aberrant conduction, but the left axis deviation and (probable) concordance point to ventricular tachycardia.
The key is the two narrow complexes near the beginning of the record: these are slightly early and are probably capture beats. They indicate that with an early supraventricular beat the conducting system can function normally; by implication, the broad complexes must be due to ventricular tachycardia.
What to do ?
An elderly patient with heart failure is more likely to have ischaemic disease than anything else, but all the possible causes of heart failure must be considered.
The sudden onset of an arrhythmia could be due to a myocardial infarction. Pulmonary emboli can cause sudden arrhythmias, though these are more often supraventricular than ventricular.
It is important to consider whether this rhythm change is related to treatment, in which case it could be due to an electrolyte imbalance or to the pro-arrhythmic effect of a drug the patient is taking.
- READ MORE:
- Similar Cases:
- ECG Case 78: Ventricular tachycardia in a 60-year-old man
- Ventricular Tachycardia with Retrograde 4:3 Wenckebach Conduction
- Ventricular Tachycardia from Cocaine Overdose
- Ventricular Tachycardia in 69 year-old man
- Idiopathic Posterior Fascicular Ventricular Tachycardia (VT)
- Hypokalemia that led to Ventricular Tachycardia (Torsades de pointes)