This article is an answer and interpretation of the ECG Case 151
Shortly after presentation, she becomes hypotensive and hypoxic and requires intubation and pressors. It was felt that she was in septic shock. it was noted that she was in acute renal failure on top of chronic renal insufficiency (previous creatinine was 2.2 mg/dL) with a creatinine that was 4.5 mg/dL.
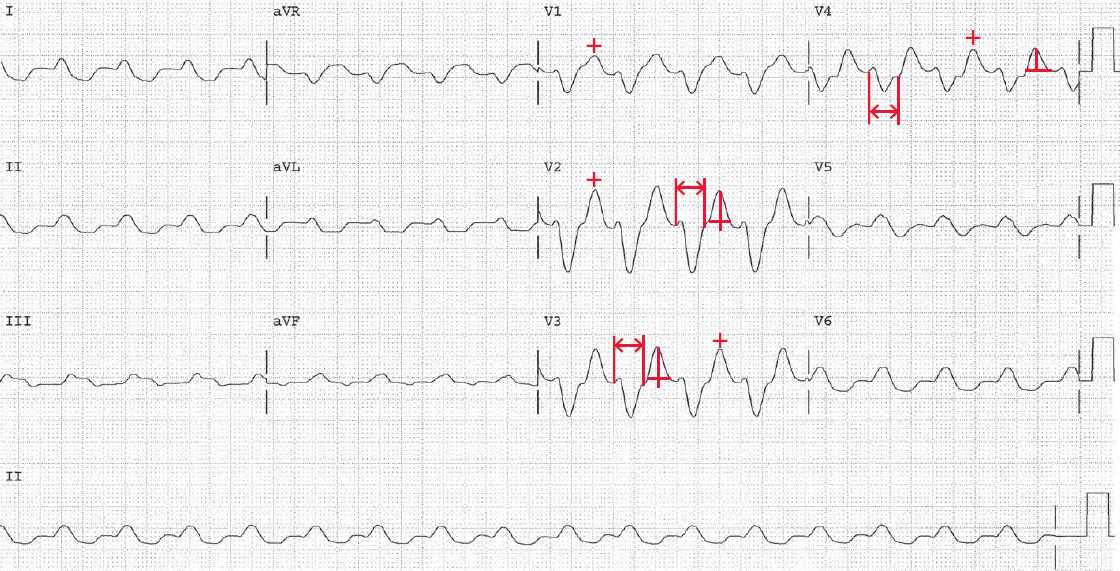
The ECG shows there is a regular rhythm with a rate of 100 bpm. There are no P waves seen before or after any QRS complexes. The QRS complex duration is very prolonged (↔) (0.28 sec). The QT/QTc intervals are prolonged (520/670 msec) but they are normal when the widened QRS complex duration is considered (360/460 msec).
The T waves (+) are symmetric, although not tall or peaked. The only condition that will prolonged the QT ≥ 0.24 sec is hyperkalemia, as a result of diffuse slowing of conduction through the His-Purkinje system.
The conduction velocity is determined by phase 0 (upstroke) of the fast action potential that is mediated by rapid influx of sodium ions. The influx rate is related to the relationship between the resting membrane potential (normal = –90 mV) and the threshold potential (–60 mV) after which a spontaneous action potential occurs.
The closer the resting membrane potential is to the threshold potential, the less rapid is the influx of sodium ions and the slower is conduction velocity. Membrane threshold potential is determined by the ratio of intracellular and extracellular potassium. Intracellular potassium concentration is much higher than the extracellular concentration.
When the extracellular potassium level increases, the resting membrane potential is less negative and hence closer to the threshold potential. Therefore, the influx of sodium ions slows and the conduction velocity decreases, causing a widening of the QRS complex duration.
The atrial myocardium is more sensitive to the effect of hyperkalemia and there is often loss of atrial activation as a result of the slowing of conduction velocity within the atrial myocardium and ultimately failure to activate the atrial myocardium. This produces atrial asystole, ie, there is still sinus node activity but no atrial activity, and hence no P wave is seen. This has been termed a sinoventricular rhythm.
Atrial asystole may occur before there is marked effect on ventricular myocardial conduction velocity and the QRS complex duration. Although there are no P waves seen, it is not clear if this is a junctional rhythm or actually sinus rhythm with the absence of atrial activation, ie, atrial asystole.
- READ MORE: ECG Interpretation – All you need to know
- SIMILAR CASES: