This article is an answer to the ECG Case 166
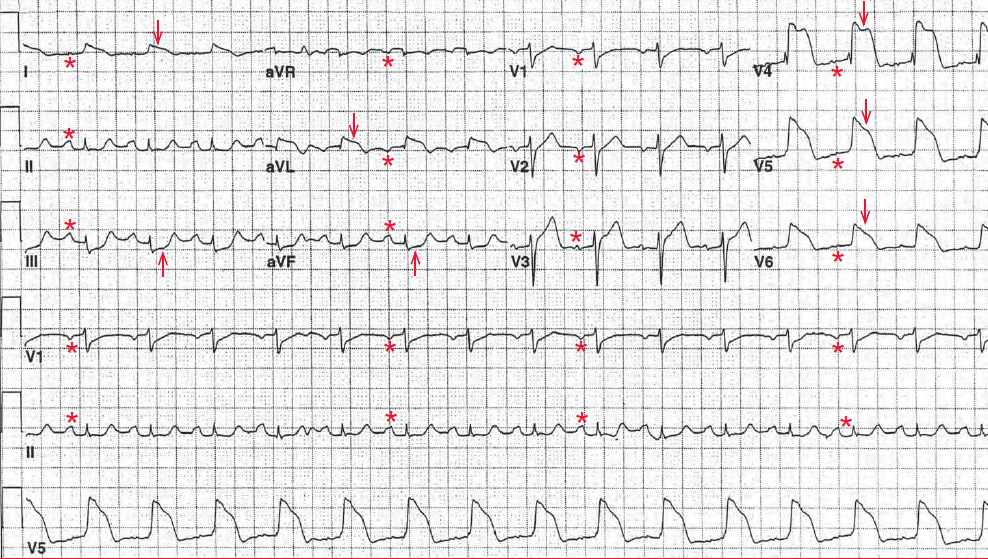
There is a regular rhythm at a rate of 90 bpm. There is a P wave (*) before each QRS complex, with a stable PR interval (0.22 sec). The P wave is negative in leads V1-V2, suggesting left atrial hypertrophy. This is a normal sinus rhythm with a first-degree AV block.
There is significant ST-segment (↓) elevation in leads I, aVL, and V4-V6, representing an acute ST-segment elevation myocardial infarction (STEMI) of the anterolateral and lateral walls.
The ST segments are convex and are merged with the T waves; there is loss of R-wave amplitude. This type of QRS complex has been termed “tombstone,” but actually the QRS complex morphology has a current of injury and resembles the fast action potential that is generated by the ventricular myocardium as a result of the rapid influx of sodium ion. This is, therefore, a monophasic action potential.
Also noted are significant ST-segment depressions (↑) in leads III and aVF, which are reciprocal changes. An acute STEMI is identified by the presence of localized ST-segment elevation, hyperacute T waves (tall, peaked, and symmetric), and reciprocal ST-segment depressions (due to the same ST-segment changes viewed from another angle or direction). The location of these changes identifies the region of the myocardium involved.
This young woman may have a coronary artery dissection, which might be due to an acute dissection of the aortic root or an isolated coronary artery dissection. Although coronary artery dissection is rare, it is an important cause of MI in young, otherwise healthy individuals.
There is a particular increase in the risk for coronary dissection in the peripartum period. It has been suggested that arterial dissection during or soon after pregnancy is related to structural changes in the intima and media of the arterial wall that are produced by hormonal and hemodynamic changes.
Although dissection can occur in the absence of risk factors, it may occur more frequently in conditions associated with hypertension that independently damage the arterial wall. The finding of spontaneous coronary artery dissection should trigger the search for a previously undiagnosed connective tissue disease, such as Marfan or Ehler-Danlos syndrome.
Unfortunately, the treatment for coronary artery dissection is difficult and complications of MI, including malignant ventricular arrhythmias and sudden cardiac death, can occur. Patients are often treated with systemic anticoagulation in order to minimize thrombosis at the site of the dissection.
There is a potential role for coronary stenting, although this is controversial. In theory, placing an intracoronary stent may stabilize the leading edge of the dissection flap, although there is a risk for stenting into the false lumen and thus propagating the dissection and jeopardizing flow through distal vessel branches.