This article is an answer to ECG Case 175
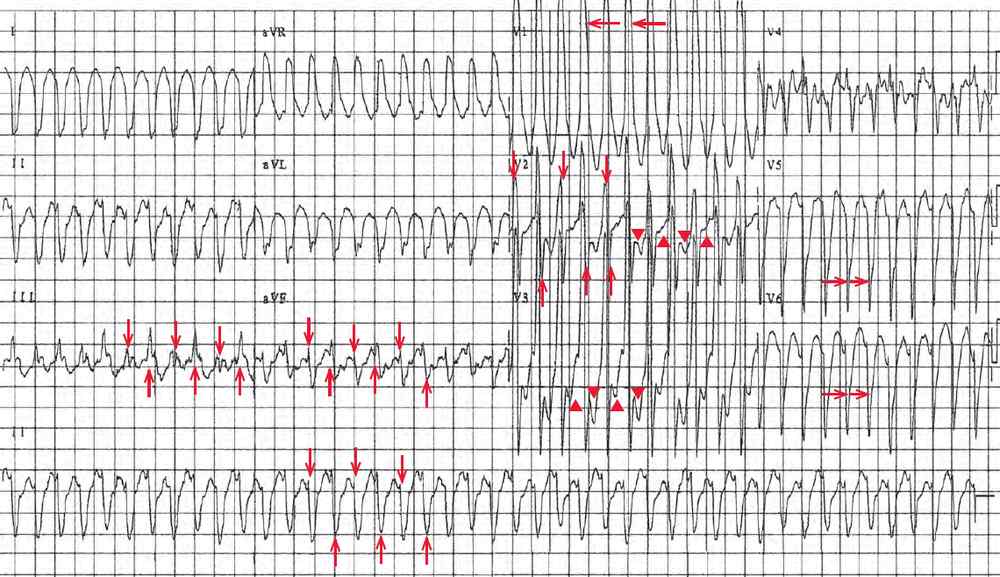
The ECG shows there is a regular rhythm with a rate of 280 bpm. There are no P waves seen before or after any of the QRS complexes. The QRS complex duration is prolonged (0.12 sec), and there is a rightward axis between +90° and +180° (QRS negative in lead I and positive in lead aVF).
The QRS complex morphology is unusual with a tall R wave in lead V1 (←), but a small R wave and deep S waves in leads V5–V6 (→). While the morphology resembles a right bundle branch block (RBBB), it is not typical. Hence this is a wide QRS complex tachycardia.
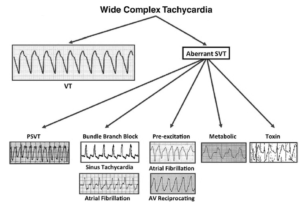
There is no obvious atrial activity. The two potential rhythms are atrial flutter with 1:1 conduction or ventricular tachycardia, which at this rate is often referred to as ventricular flutter.
The fact that the patient has known congenital heart disease does not help establish a diagnosis. However, there are beat-to-beat changes in QRS amplitude (↓, ↑). This is termed electrical or QRS alternans. There are also beat-to-beat changes in the T waves (▲, ▼) that are T-wave alternans.
The presence of electrical (or QRS) and T-wave alternans is more suggestive that this is a supraventricular tachyarrhythmia, and likely flutter with 1:1 AV conduction. Although it has been reported that electrical alternans may occur in ventricular tachycardia, this is very unusual. It may be more frequently seen in a right ventricular outflow tachycardia or a fascicular tachycardia, which is a type of ventricular tachycardia in which one of the fascicles (most often the left posterior fascicle) is part of the circuit of the tachycardia.
The QRS complex morphology is not typical for a right ventricular outflow tachycardia (which has a left bundle branch block morphology and a normal axis). Fascicular tachycardias are not usually this rapid, although the right axis and RBBB morphology does suggest a possible left anterior fascicular tachycardia, which is far less common. Therefore, the most likely diagnosis is atrial flutter, with an unusual QRS complex morphology as the result of underlying congenital heart disease. The morphology is suggestive of right ventricular hypertrophy.
QRS and T-wave alternans in atrial flutter with a rapid ventricular rate is a result of beat-to-beat changes in calcium influxes into the ventricular myocardium. It may occur with any rapid supraventricular tachycardia, including atrial tachycardia, atrial flutter, atrioventricular nodal reentrant tachycardia (AVNRT), or atrioventricular reentrant tachycardia (AVRT) as occurs with a preexcitation syndrome.
Electrical alternans due to the same mechanism may be seen in a dilated cardiomyopathy, decompensated heart failure, or an acute myocardial infarction. It is also seen with cardiac tamponade as the result of the heart swinging with each beat in a fluid-filled pericardial sac (pendulum effect). In this situation, there is QRS and T-wave alternans present, and there may also be P-wave alternans.
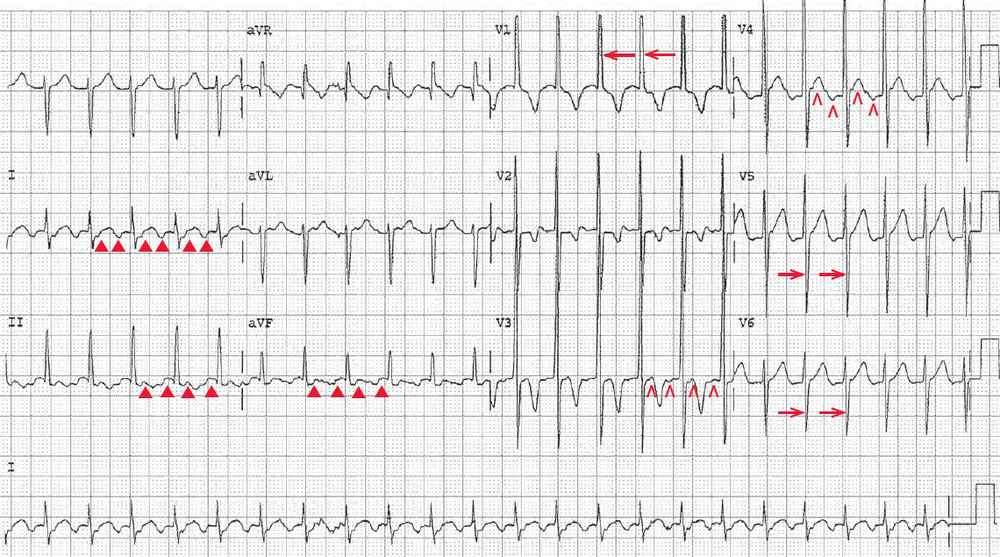
Several minutes after presentation, the heart rate abruptly slowed to 140 bpm, and another ECG was obtained.
There is a regular rhythm with a rate of 140 bpm. Although there are no distinct P waves, there are typical atrial flutter waves (at a rate of 280 bpm) seen, primarily in leads II, III, and aVF (▲). They may also be seen in leads V3–V4 (^). Hence this rhythm is atrial flutter with 2:1 AV block. The atrial rate is identical to the ventricular rate in the previous ECG, confirming that this was indeed atrial flutter with 1:1 AV conduction.
There is a tall R wave in lead V1 (←) and a deep S wave in leads V5–V6 (→), with an S/R ratio > 1. The tall R wave in V1 and the deep S wave in leads V5–V6 are characteristic for right ventricular hypertrophy; this accounts for the rightward axis. Although the nature of the congenital heart disease is not certain, it was most certainly associated with right ventricular volume or pressure load, and most likely due to left to right shunting.