This article is an answer to the ECG Case 178
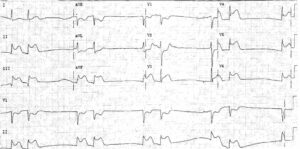
The rhythm strip shows a wide complex tachycardia at a rate of 240 bpm. There are no obvious P waves noted. This is a rapid ventricular tachycardia. It can be seen that the cardioverter/defibrillator delivered a nonsynchronized shock. The energy used was only 50 joules.
The electric shock was delivered on the T wave (↑) and resulted in ventricular fibrillation. This is the same as the R-on-T phenomenon.
The use of an electric shock to treat arrhythmias is either defibrillation or cardioversion.
Defibrillation is the nonsynchronized delivery of energy, ie, the shock is not related to the QRS and is delivered as soon as the button on the machine is pushed. Hence the discharge may occur at any time during the cardiac cycle. In general, high energy levels are required with defibrillation to make certain that an adequate amount of energy reaches the heart so that the entire myocardium is depolarized simultaneously. Often the maximum output of the machine is used, ie, 360 joules with a monophasic waveform and 200 joules with a biphasic waveform.
Cardioversion is the synchronized delivery of energy, ie, the shock is coupled to the cardiac cycle and is delivered simultaneously with the R wave; hence the shock is delivered when the myocardium is already depolarized and hence less energy is required to insure that all of the myocardium is depolarized, especially the reentrant circuit responsible for the arrhythmia.
Defibrillation (with high energy) is the preferred method for delivering an electric shock to depolarize the ventricular myocardium when distinct QRS complex are not present (as with ventricular fibrillation) or when there is no distinct R wave and the QRS complex cannot be distinguished from the T wave. If cardioversion is used in this situation, there is an equal chance for the electrical discharge to be delivered on the R wave or the T wave.
When a distinct R wave can be identified, cardioversion should be used, as the termination of an arrhythmia occurs with lower energy levels. When the machine is set to defibrillation, a nonsynchronized shock is delivered, ie, the shock occurs as soon as the button on the machine is pushed. Hence the shock may be delivered at any time during the cardiac cycle.
If there is a distinct QRS complex and T wave, there is the possibility of delivering a shock on the T wave that has a potential to provoke ventricular fibrillation if a low energy shock is used.
The T wave corresponds to the vulnerable period of the action potential and is a time when the membrane potential is more negative than the resting membrane potential (ie, less negative than –90 mv). This is the time during the action potential that the ventricular fibrillation threshold is determined. Generally, a relatively high energy level is necessary to provoke ventricular fibrillation. However, with ischemia the threshold is lower, and even a low energy impulse can provoke ventricular fibrillation.
Therefore, in this case the use of low-energy defibrillation (50 joules) delivered the shock on the T wave, resulting in ventricular fibrillation. In this patient, distinct QRS complexes are seen (+) and cardioversion (delivery of energy synchronous with the QRS complex) should have been used. Since defibrillation was used, a higher energy level would have been more appropriate.
READ MORE: ECG Interpretation – All you need to know