This post is answer to the ECG Case 220
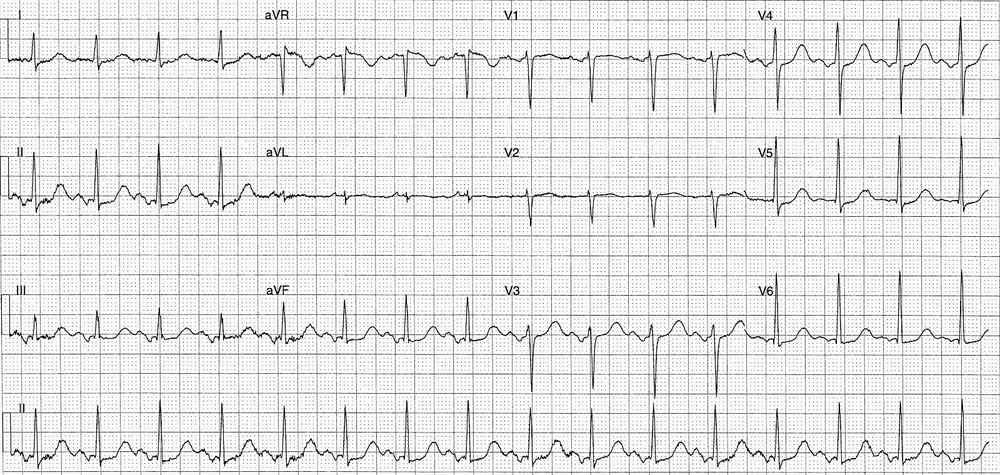
ECG 1 – Initial ECG on arrival to the Emergency Department
- Rate:
- ~220 bpm
- R-R Interval ~280ms
- Rhythm:
- Regular
- Nil p wave visible
- Axis: Extreme Axis deviation
- Intervals: QRS – Prolonged at 120ms
- Additional:
- Precordial transistion in lead V6
- Extensive artifact obscures lead I
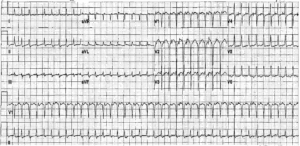
ECG 2 – Performed shortly after ECG 1 and prior to treatment.
- Rate: 220 bpm
- Rhythm:
- Regular
- Nil P waves visible
- Axis: LAD (-45 deg)
- Intervals:
- QRS – Normal (80ms)
- QT – 280ms
- Segments:
- ST Elevation in aVR (2.5mm)
- ST Depression in leads I, II, III, aVF, V4-6
- Additional:
- Notching of terminal QRS / early ST segment best seen in leads II, III, V6
Interpretation
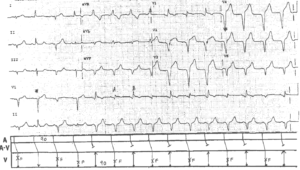
AVNRT with rate related LBBB in the first ECG (Differential Diagnosis of Atrial flutter with 1:1 conduction).
ST segment changes related to dysrythmia rate or ischaemic pattern of potential left main or severe multi-vessel disease.
What happened next ?
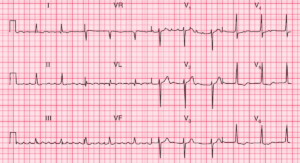
The patient underwent DC cardioversion under procedural sedation with reversion to sinus rhythm, post cardioversion ECG below.
Despite no chest pain the post cardioversion ECG shows infero-lateral ST segment depression with ST elevation in aVR, the patient’s troponin peaked at 1.4 [Normal <0.05]. An angiogram was performed which showed:
- LAD: 50% Stenosis
- Cx: 60% Stenosis
- RCA: 30% Stenosis
The patient underwent a cardiac ablation following this episode.
READ MORE: Never Mistake Ventricular Tachycardia for Supraventricular Tachycardia with Aberrant Conduction