This post is an answer to the Case – Patient with Swollen Leg and Skin Change
What names are given to this common condition?
The popular term is varicose ulcer, which is often a misnomer, as will be discussed below. Other names are venous ulcer or gravitational ulcer.
On examination, there was no evidence of varicose veins on either leg, so what is the likely aetiology of the ulcer in this patient?
A preceding deep vein thrombosis (presumably complicating her last pregnancy). This would have caused damage to the valves of the deep veins in her leg, which would have resulted in venous hypertension and, therefore, poor cutaneous blood supply to the skin and subcutaneous tissues of the lower leg.
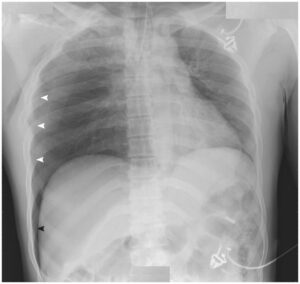
What do you notice about the patient’s foot and the skin surrounding the ulcer? Can you explain these changes?
The foot is oedematous as a result of the venous hypertension in the lower leg (remember Starling’s law of fluid exchange in the tissues). The skin surrounding the ulcer shows the typical pigmentation, often called ‘varicose eczema’, which results from diapedesis of red cells through the capillaries. These break down and deposit haemosiderin in the soft tissues.
What is a dangerous, but fortunately uncommon, complication of longstanding cases of this disease?
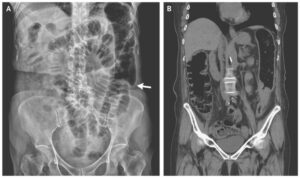
Malignant change at the edge of the ulcer into a squamous carcinoma – an example of a Marjolin’s ulcer* (malignant change in any chronic ulcer). Indeed, we were suspicious that this might have taken place at the lower edge of this woman’s ulcer, but a tissue biopsy revealed no evidence of tumour. A clinical feature that suggests malignancy is a non-healing ulcer with a raised margin, particularly one that has shown a recent unexplained deterioration in appearance.
What are the other possible causes of a chronic ulcer of the leg?
Venous ulcers are by far the commonest cause of a chronic ulcer of the leg in the Western world, and account for about 90% of cases. However, it is important to remember that other causes occur, whose treatment and prognosis may be very different. These can be listed as follows:
- Venous ulcer: Complicating deep venous insufficiency.
- Ischaemic ulcer: Due to impaired arterial blood supply; the peripheral pulses must always be examined and the ankle–brachial pressure index (ABPI) checked.
- Neuropathic ulcer: Particularly common in diabetics, where it is often compounded by ischaemia due to diabetic microangiopathy.
- Malignant ulcer: A squamous carcinoma, often arising in a pre-existing chronic ulcer or an ulcerated malignant melanoma.
- Ulcer complicating systemic disease, e.g. acholuric jaundice, ulcerative colitis and rheumatoid arthritis
- Arteriovenous fistula-associated ulcer.
- Repetitive self-inflicted injury.
- Gummatous ulcer of syphilis: Usually affects the upper one-third of the leg.
How should this patient be treated?
A number of important steps are taken:
- She is advised to keep the leg elevated whenever possible – in bed at night and when sitting during the day. The foot should be higher than the knee, the knee higher than the hip. This eliminates the venous hypertension in the leg during the hours the leg is elevated and allows ingress of oxygenated blood.
- All ointments and medicaments should be thrown away.
- The ulcer is covered with a simple, non-adherent dry dressing, held in place by a paste bandage to the leg, and over this elastoplast bandaging is applied from the toes to below the knee. Again, this counters the venous hypertension. The bandages are changed initially at weekly intervals, but as healing progresses and the amount of oozing is reduced the intervals between dressings can be increased.
- A split-skin graft can be applied if the ulcer remains indolent.
- Once the ulcer is healed, elastic stocking support is mandatory to prevent the very real risk of recurrence.