This post is an answer to the Case – Tongue Deviation
Cranial computed tomography revealed dilatation of the ventricular system and diffuse cerebral edema, which had caused collapse of the basal cisterns. A lumbar puncture yielded purulent cerebrospinal fluid with positive cultures for Neisseria meningitidis.
An external ventricular drain was placed, and treatment with 4 g of ceftriaxone per day was initiated. Ventricular drainage was successfully withdrawn 9 days after admission.
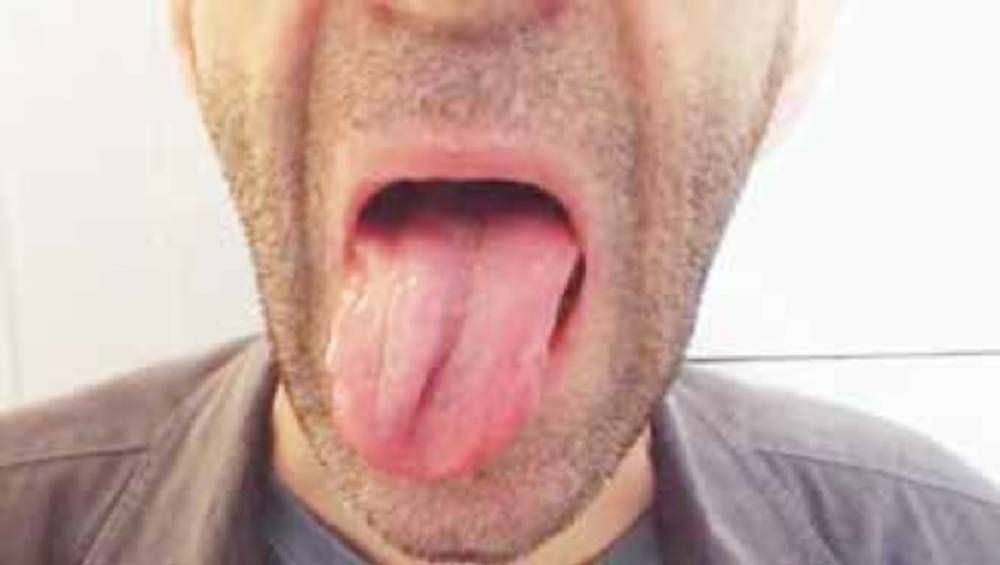
The patient also had palsy of the right hypoglossal nerve (cranial nerve XII). Although he had generalized weakness, no other focal motor signs or deafness were apparent. At follow-up 5 months after discharge, the patient had gained weight and was in good health, including spontaneous resolution of the nerve palsy.
Cranial nerve palsies, which occur in 5 to 10% of adult patients with bacterial meningitis, are mostly a result of compression caused by brain swelling or of perineuritis caused by meningeal inflammation.
The nerves most frequently affected are cranial nerves III, IV, VI, and VII, and the palsies are usually permanent. Palsies in other cranial nerves are usually transient, as was the case in our patient.