This article is an answer to the Case – Uremia and Shortness of Breath
Radiologic Findings
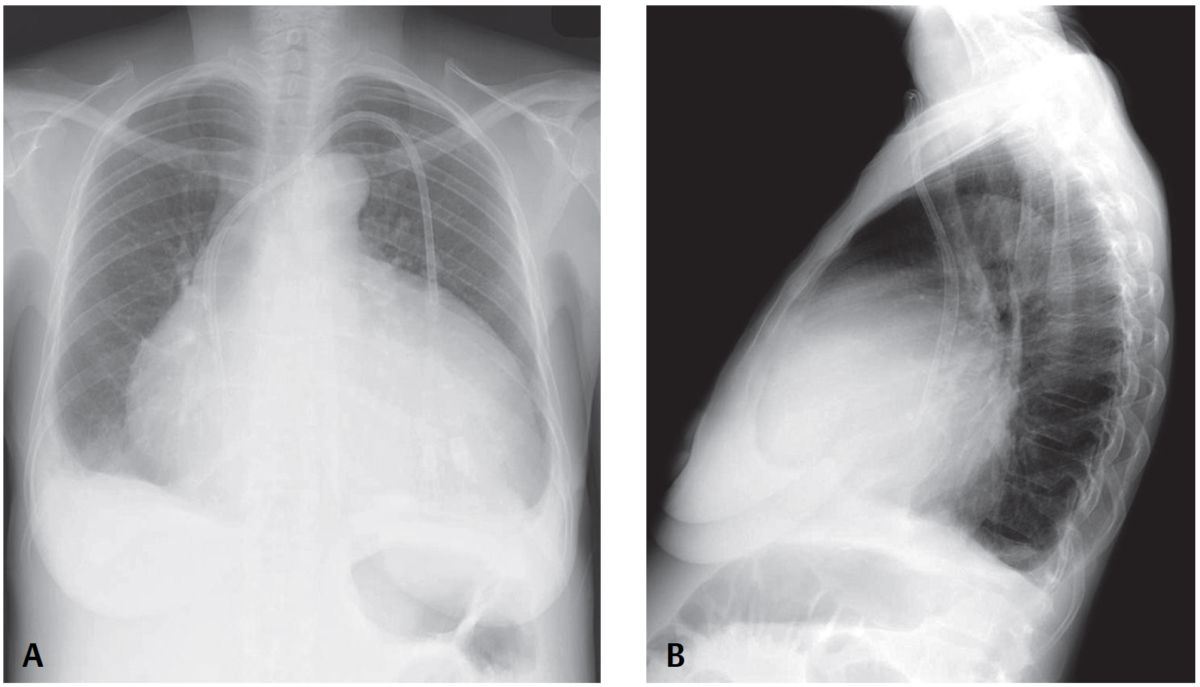
PA chest X-ray reveals an enlarged cardiomediastinal silhouette with an increase in the transverse diameter but no increase in its height, and straightening of the upper mediastinal borders, creating a globular or water bottle morphology (water bottle sign). The vascular clarity is slightly diminished and bilateral pleural effusions are present, right greater than left.
Lateral exam also shows globular enlargement of the cardiomediastinal silhouette and separation of the outer retrosternal and inner epicardial fat lines—fat pad or Oreo cookie sign).
Diagnosis
Pericardial Effusion
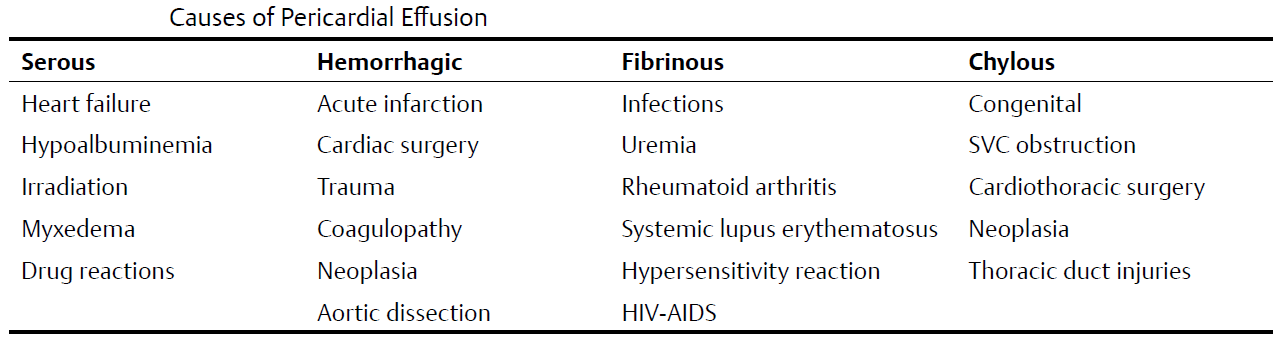
Differential Diagnosis
Global Cardiomegaly—Cardiomyopathy
Etiology
Increased volumes of pericardial fluid and alterations in the composition of normal pericardial fluid may occur in the setting of numerous diseases.
Clinical Findings
Patients may have a relatively large pericardial effusion and experience little or no clinical signs or symptoms, particularly if the fluid has increased slowly over time. This more commonly occurs when the pericardial effusion is the result of neoplasia or a chronic inflammatory disorder (e.g., rheumatoid arthritis).
Alternatively, patients with pericardial effusion may experience dyspnea, orthopnea, both pleuritic and non-pleuritic chest pain, cough, syncope or near syncope, fatigue, tachycardia, and low-grade fever. Tamponade occurs when the volume of pericardial fluid compromises blood return to the right heart, affecting cardiac output, and is usually caused by serous or bloody fluid.
Imaging Findings
Chest Radiography
- Normal until volume of fluid >250 mL
- Increased transverse dimension of cardiomediastinal silhouette (water bottle sign) (80% specific; 46% sensitive)
- Enlargement of cardiomediastinal silhouette compared with antecedent chest exams (41% specific; 71% sensitive)
- Separation of retrosternal and epicardial fat stripe >2 mm (fat pad or Oreo® cookie sign) (94% specific; 12% sensitive); seen best with moderate-large pericardial effusions
- Cardiomegaly with normal pulmonary vascular clarity
- Left pleural effusion (100% specific; 20% sensitive)
MDCT
- Small effusions first collect dorsal to left ventricle and along left atrium
- Larger effusions collect ventral and lateral to right ventricle
- Even larger effusions may envelop the myocardium (halo sign)
- Loculations most often form along right anterolateral pericardium
MRI
- Similar morphologic features to those depicted on CT
- Transudates: low signal intensity T1WI
- Exudates: higher signal intensity T1WI
- Cine sequences may reveal hemodynamic consequences of pericardial effusion; compression/deformity of right atrium is of hemodynamic significance
Management
- Directed toward underlying cause
- Pericardiocentesis or pericardial window when clinically necessary
Prognosis
Dependent upon underlying cause
Pearls
- Echocardiography is the modality of choice for detecting pericardial effusion, although CT and MRI are more sensitive for detection of smaller-volume effusions.
- Reliable distinction between benign and malignant pericardial effusion is not possible on the basis of Hounsfield units alone.
Suggested Reading
- Eisenberg MJ, Dunn MM, Kanth N, Gamsu G, Schiller NB. Diagnostic value of chest radiography for pericardial effusion. J Am Coll Cardiol 1993;22(2):588–593
- Wang ZJ, Reddy GP, Gotway MB, Yeh BM, Hetts SW, Higgins CB. CT and MR imaging of pericardial disease. Radiographics 2003;23(Spec No):S167–S180