This article is an answer to the Case – Post Hysterectomy for Uterine Cancer
Radiologic Findings
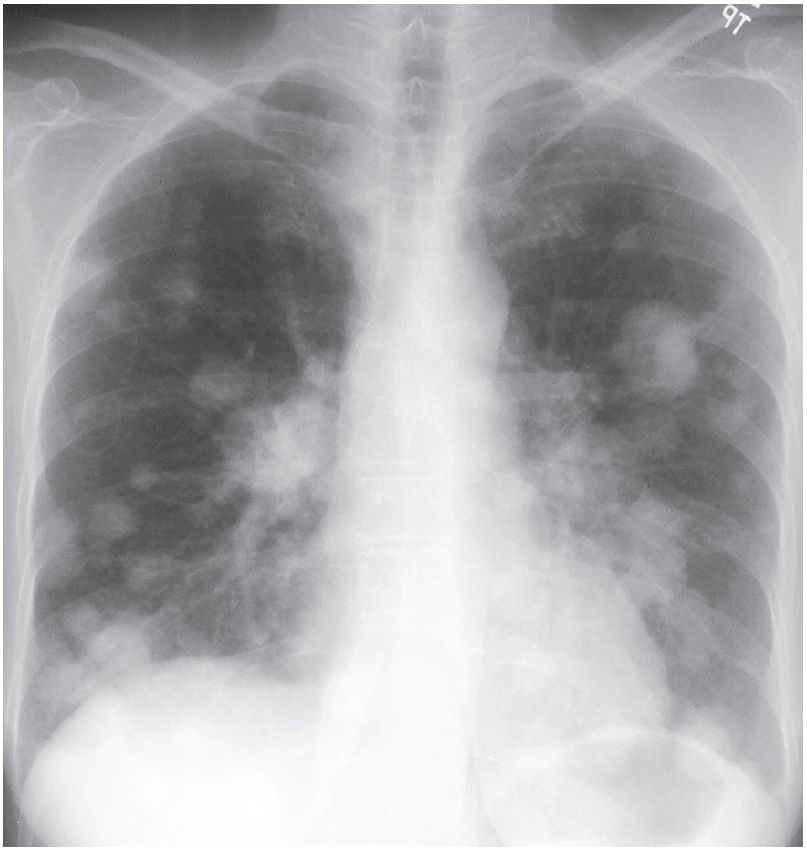
Chest radiographs demonstrate multiple bilateral well-defined spherical pulmonary nodules and masses, which are most numerous in the lung bases.
Differential Diagnosis
- Primary Pulmonary Lymphoma
- Multicentric Lung Cancer
- Hematogenous Infection
- Vasculitis
Background
The term metastasis is generally defined as the transfer of disease from one organ to another that is not in direct contiguity. In the setting of neoplasia, metastases are characteristic of malignancy.
Pulmonary metastases represent the most frequent pulmonary neoplasm. Depending on the location of the primary tumor, lung metastases may represent early or late neoplastic dissemination. Secondary lung neoplasia may occur via hematogenous, lymphatic, and tracheobronchial routes.
Etiology
Pulmonary metastases typically result from hematogenous dissemination of malignancy. The neoplastic cells are transported to the lung and “arrest” in its capillary bed. Thus, most primary neoplasms that produce lung metastases have a rich vascular supply and a venous drainage into the systemic circulation, with the lung as the filtering organ. Pulmonary metastases may in turn metastasize and produce disseminated malignancy.
Clinical Findings
Patients with pulmonary metastases may be entirely asymptomatic. When metastases are numerous, large, and/or involve the airways and pleura, affected patients may experience dyspnea, cough, chest pain, and respiratory failure.
Patients with lymphangitic carcinomatosis typically present with dyspnea. Patients with sarcoma metastatic to the lung may present with acute chest pain because of secondary spontaneous pneumothorax.
Most patients with pulmonary metastases have a known history of malignancy. Rarely, patients present with pulmonary metastases from an unknown primary neoplasm.
Imaging Findings
Chest Radiography
- Bilateral multifocal well-defined nodules/masses; spherical morphology
- Variable size (miliary nodules to large cannon ball masses)
- Multi-focal opacities with ill-defined borders; may mimic air space disease
- Most numerous in the lower lobes
- May exhibit associated hilar/mediastinal lymphadenopathy
- May exhibit associated pleural effusion
- Rarely:
- Cavitation, most frequent in metastases from squamous cell carcinomas, but also described in adenocarcinomas and sarcomas
- Calcification
- Solitary nodule/mass
- Endobronchial lesion; may exhibit atelectasis/consolidation
- Lymphangitic carcinomatosis
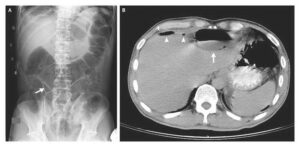
MDCT
- Multi-focal well-defined spherical pulmonary nodules/masses
- Variable shape; larger nodules may be lobular or exhibit irregular margins
- Most numerous in lung bases and subpleural lung periphery (outer one-third of lung)
- May exhibit associated lymphadenopathy and/or pleural effusion
- May exhibit a vascular relationship (angiocentric), a pulmonary vessel coursing into the metastasis (feeding vessel sign)
- Rarely
- Cavitation
- Calcification (e.g., osteogenic sarcoma, synovial cell sarcoma, or chondrosarcoma metastases)
- Solitary nodule/mass
- Lymphangitic carcinomatosis
- Endobronchial metastases
- Intravascular tumor emboli (most commonly hepatocellular carcinoma; adenocarcinoma of breast and stomach)
Management
- Systemic therapy based on cell type
- Radiation therapy in selected cases
- Surgical excision of solitary or limited pulmonary metastases (when the lung is the only affected site) with continued surveillance and possible additional metastasectomies
- Radiofrequency ablation
Prognosis
- Poor
- Better in patients with limited metastases who are candidates for metastasectomy
Pearls
- CT is more sensitive than radiography in detecting pulmonary metastases, particularly for nodules over 3 mm in size. However, it is also less specific as it detects unrelated benign, previously unsuspected pulmonary nodules. The likelihood of benign disease increases when pulmonary nodules are detected only on CT.
- Solitary pulmonary metastases are rare. Thus, lung cancer must always be included in the differential diagnosis of a patient with known malignancy who presents with a new solitary pulmonary nodule or mass. Solitary metastases typically result from sarcomas, melanoma, or colon, breast, and genitourinary cancers. A new solitary nodule in a patient with known invasive melanoma or skeletal sarcoma is more likely to represent a metastasis. A new solitary nodule in a patient with known squamous cell carcinoma or lymphoma is more likely to represent a new primary lung cancer.
- Patients with endobronchial metastases may exhibit findings of bronchial obstruction (pneumonia, atelectasis) mimicking the presentation of central lung cancer.
- Differential diagnosis for Cannonball metastases includes colorectal, renal cell, and breast carcinomas; sarcoma; seminomatous and non-seminomatous germ cell tumors; melanoma; follicular thyroid cancer.
Suggested Reading
- Aquino SL. Imaging of metastatic disease to the thorax. Radiol Clin North Am 2005;43(3):481–495, vii
- Gillams AR, Lees WR. Radiofrequency ablation of lung metastases: factors influencing success. Eur Radiol 2008; 18(4):672–677
- Seo JB, Im JG, Goo JM, Chung MJ, Kim MY. Atypical pulmonary metastases: spectrum of radiologic findings. Radiographics 2001;21(2):403–417